


Introduction
You might work through this system over several weeks, days or hours, but to enhance your learning and enjoyment make sure you break it up into bite-size chunks. Here are the sections of the cardiovascular system:
Make notes as you study each section, and interact fully with the activities – watch the animations and complete the quizzes.
Take a break at the end of each section– resting your eyes from the computer screen, getting some fresh air or taking a coffee break will improve your ability to focus on your study and take in information.
Give yourself time to think about what you have learned, and time to absorb and understand it.
UHI / CC0
The cardiovascular system
As you study the cardiovascular system you will learn about:
- Structure of the heart
- Blood flow through the heart
- The heart beat
- Heart rate
- Blood pressure
- Blood vessels
- Blood
UHI / CC0
Superior vena cava
Pulmonary veins
Pulmonary artery
Pulmonaryvalve
Left atrium
Right atrium
Biscupid valave
Triscupid valve
Left ventricle
Right ventricle
Myocardium
Pedicardium
Septum
Structure and functions of the cardiovascular system
Structure of the cardiovascular system
The cardiovascular system is comprised of three components:
- A pump (the heart)
- A system of channels (blood vessels)
- A fluid medium (blood)
Our cells need a constant supply of oxygen and nutrients, which are obtained via the cardiovascular blood supply. Cells also expel waste products such as carbon dioxide back into the capillaries carrying the blood to be returned to the heart and lungs.
Functions of the cardiovascular system
The cardiovascular system:
- Delivers oxygen and nutrients to every cell in the body
- Transports hormones from endocrine glands to their target receptors
- Removes carbon dioxide and metabolic waste products from cells and tissues
- Maintains body temperature, fluid levels and appropriate internal pH levels
- Limits tissue damage and prevents infection from invading organisms.
Systematic and pulmonary circulation
There are two closed circulatory systems:
- The pulmonary system
- The systemic system
The left side of the heart pumps oxygenated blood via the aorta (large artery) to the body (systemic circulation), and the right side of the heart pumps de-oxygenated blood via the pulmonary artery to the lungs (pulmonary circulation).
The heart is shown as if you were viewing it in the body, so the left atrium and ventricle appear on the right hand side in diagrams, and the right atrium and ventricle appear on the left.
UHI / CC0
(Click image to toggle animation on/off)
Pulmonary artery
Right atrium
Vena cavae
Right ventricle
Pulmonary vein
Left atrium
Aorta
Left ventricle
The heart
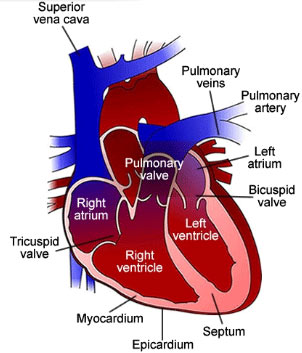
The heart is approximately the size of a closed fist, and is located inside the ribcage between the lungs, sitting in the cardiac notch of the left lung. It is divided into four chambers, each surrounded by muscle tissue (myocardium):
- Right atrium
- Left atrium
- Right ventricle
- Left ventricle
The two atria are located above the ventricles. Walls of connective tissue separate the chambers from each other: the interatrial septum separates the atria, and the interventricular septum separates the ventricles. These walls are collectively known as the septum.
The thickness of the chamber walls varies according to their function. The atria need to pump blood only into the ventricles; the ventricles have to pump blood through the body, so they have thicker, more muscular walls.
Although the ventricles expel the same blood volume, the left ventricular wall is 2-4 times thicker than that of the right ventricular wall, as it has to pump blood to the body via the systemic circulation. The right ventricle pumps blood to the lungs via the pulmonary circulation.
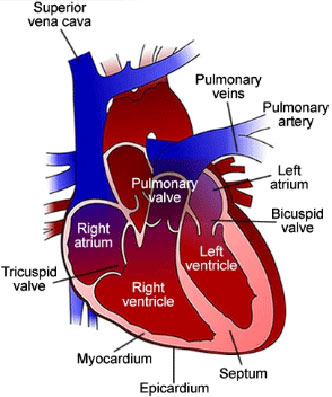
UHI / CC0
Superior vena cava
Pulmonary veins
Pulmonary artery
Pulmonary valve
Left atrium
Right atrium
Biscupid valave
Triscupid valve
Left ventricle
Right ventricle
Myocardium
Pedicardium
Septum
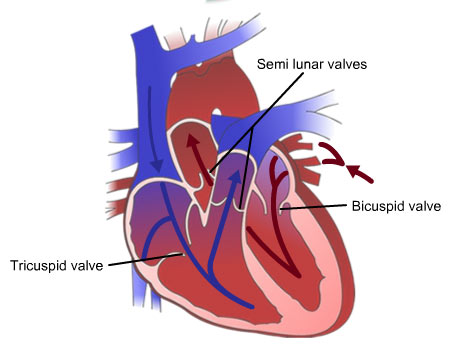
Valves of the heart
Valves made of dense connective tissue are present between the atria and ventricles to prevent backflow into the atria. The valve between the right atrium and ventricle is the tricuspid valve (it has three cusps). The biscuspid, or mitral valve between the left atrium and left ventricle has two cusps. Valves which lie between the atria and ventricles may also be called atrioventricular (AV) valves.
Blood moves from the atria into the ventricles through open AV valves when ventricular pressure is lower than atrial pressure. When the ventricles contract, the pressure of the blood closes the valves. If any of the valves are damaged then blood may regurgitate into the atria when the ventricles contract.
Semi lunar valves in the pulmonary artery and aorta also prevent back flow; if blood begins to flow back into the heart, it will fill the cusps and close the valve. The arrows in this diagram show the direction of blood flow into and out of the heart.
Connective tissues of the heart
The heart is enclosed within a triple-layered sac called the pericardium. The outer fibrous layer is made of tough, dense connective tissue and is lined with a double layer of membrane. The inner membrane of the pericardium is also known as the epicardium, which adheres to the surface of the heart and forms the first of three layers of the heart wall.
Epicardium (outer layer) – connective tissue on the outside of the heart wall
Myocardium (middle layer) – cardiac muscle tissue which makes up most of the heart and enables its pumping action
Endocardium (inner layer) – a thin membrane covering the heart valves and lining the inside of the heart. It is continuous with the endothelial lining of the large blood vessels and the rest of the cardiovascular system.
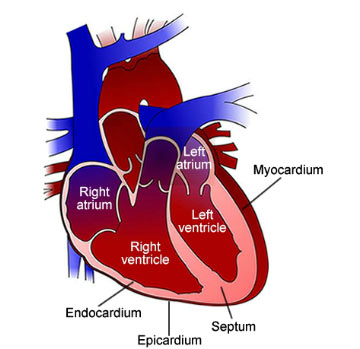
UHI / CC0
Left atrium, right atrium, left ventricle, right ventricle.
Myocardium, Endocardium, Epicardium, Septum.
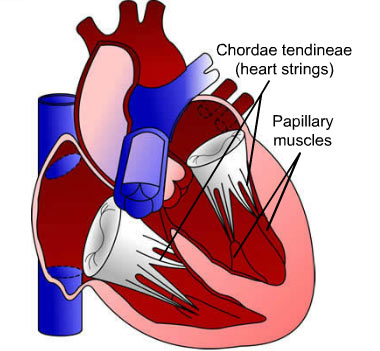
Chordae tendineae and papillary muscles
The chordae tendineae (heart strings) are strips of connective tissue (tendons) that connect the bicuspid and tricuspid valves to the papillary muscles in the heart.
When the right and left ventricles contract and blood pressure increases, the papillary muscles contract and tighten the chordae tendineae, preventing the flaps from being inverted into the atria. Regurgitation of ventricular blood back into the atrial cavities is thus prevented.
Quiz
Move the labels on either side of the image using your mouse to name the different areas of the heart.
The coronary sinus
Remember, the circuit of blood flow from the heart to the lungs and back is known as pulmonary circulation; blood flow from the left ventricle via the aorta to the body and back is known as systemic circulation.
A third circulatory system serves the heart itself.
The coronary sinus is a collection of veins meeting in the right atrium that collects blood from the myocardium. It delivers deoxygenated blood from the cardiac tissues into the right atrium.
Some small veins drain into any of the heart chambers directly.
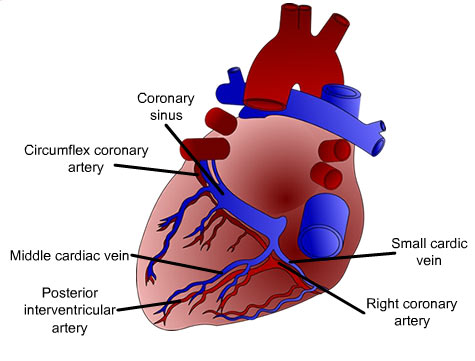
UHI / CC0
Coronary sinus
Circumflex coronary artery
Middle cardiac vein
Posterior interventricular artery
Small cardic vein
Right coronary artery
Blood flow through the heart
Blood flows back to the heart from the body via the inferior and superior vena cavae. It is de-oxygenated and is pumped out to the lungs via the pulmonary artery to become oxygenated. It returns to the heart via the pulmonary vein, and is pumped out to the body via the aorta.
The pulmonary artery is the only artery in the body that carries deoxygenated blood. All other arteries carry oxygenated blood, but this blood vessel is carrying blood from the heart (which is why it is an artery), to the lungs to become oxygenated. Veins carry deoxygenated blood, but the pulmonary vein is returning oxygenated blood to the heart from the lungs, so the pulmonary artery and pulmonary vein in the pulmonary circuit are different from other arteries and veins in the systemic circulation.
UHI / CC0
(Click image to toggle animation on/off)
Pulmonary artery
Right atrium
Vena cavae
Right ventricle
Pulmonary vein
Left atrium
Aorta
Left ventricle
The right atrium receives deoxygenated blood from the body via the inferior (lower) and superior (upper) vena cava.
From the right atrium the blood flows through the tricuspid valve and into the right ventricle, which pumps the blood into the pulmonary trunk.
The pulmonary trunk divides into a right and left pulmonary artery carrying blood to the lungs.
As blood flows through the pulmonary capillaries around the alveoli in the lungs, it loses carbon dioxide and takes on oxygen. The left atrium receives oxygenated blood from the lungs via the pulmonary vein.
From the left atrium the blood flows through the bicuspid valve and into the left ventricle, which pumps the blood into the aorta. The aorta delivers oxygenated blood to the body through arteries and capillaries. As it flows through the capillary network, it loses oxygen and gains carbon dioxide.
The de-oxygenated blood from the body cells returns to the right hand side of the heart via the inferior and superior vena cava. The inferior vena cava brings blood from parts of the body below the diaphragm, the superior vena cava from parts above it.
Quiz
The heartbeat
During foetal development a small number of cardiac muscle fibres become autorhythmic (self-excitable) and able to generate action potentials. These fibres act as a pace maker and create the pattern of contraction that we know as our heartbeat.
The heartbeat originates from the sinoatrial node (SA node) in the right atrium. Myocardial muscle cells contract, sending a signal to other atrial muscle cells to contract.
The signal spreads to the atrioventricular node (AV node) in the septum between the atria. The action potential continues from the AV node to the Bundle of His, (atrioventricular (AV) bundle), the only electrical connection between the atria and ventricles, and travels down right and left branches towards the bottom (apex) of the heart, finally reaching the Purkinje fibres and causing the ventricles to contract simultaneously.
After the action potential (excitation) is received in the cardiac fibres, muscular contraction follows shortly afterwards due to the movement of calcium ions and their interaction with contractile proteins actin and myosin (you will learn more about these when you study the muscular system). Blood flow through the heart occurs as a result of these muscular contractions.
UHI / CC0
(Click image to toggle animation on/off)
SA node, AV node, Bundle of HIS, Purkinje fibres
The pacemaker and automatic control of the heart
The specialized muscle fibres in the sinoatrial (SA) node initiate action potentials at a rate of 90 to 100 times per minute. This is faster than action potentials that may be initiated from other areas, so the SA node stimulates other areas of the conduction system first so that they do not create their own slower electrical signal. The electrical message from the SA node is therefore the pacemaker, although if these fibres become damaged, cells in the AV node (the secondary pacemaker) take over and usually create 40-60 beats per minute. However, heart rate is constantly modified by sympathetic and parasympathetic nerve fibres, and the average resting heart rate in adult humans is approximately 70 beats per minute.
The heart beat and heart rate
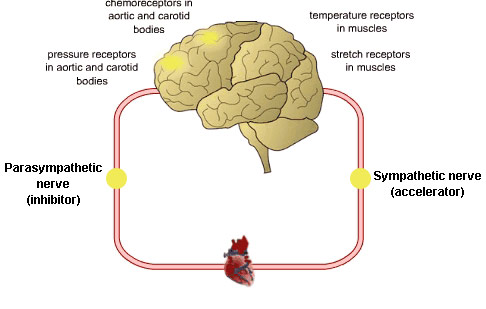
The cardiovascular centre in the medulla oblongata, located in the brain stem, receives information from other areas of the brain and body, and conveys the relevant nervous output to the heart via the sympathetic and parasympathetic branches of the autonomic nervous system (ANS).
The sympathetic nervous system increases the heart rate and stroke volume in response to a number of different messages from other parts of the body. The sympathetic nervous system is stimulated during exercise, stress, anger, fear or emotion, with an end result of increased cardiovascular output.
During exercise, chemoreceptors register the increased amount of carbon dioxide (CO2) and reduced blood pH, and send this information to the cardiovascular centre in the brain. Sympathetic nerve fibres send a message on to the SA node and myocardium, increasing cardiac output through increased depolarization in the SA and AV nodes (increasing heart rate) and increasing atrial and ventricular contractility (increasing stroke volume). This pumps more blood to the lungs so the CO2 can be exhaled and blood pH returns to normal.
UHI / CC0
(Click image to toggle animation on/off)
Parasympathetic nerve (inhibitor), pressure receptors in aortic and carotid bodies, chemoreceptors in aortic and carotid bodies, temperature receptors in muscles, stretch receptors in muscles, Sympathetic nerve (accelerator).
How the nervous system affects our heart rate
Sympathetic impulses cause an increase in heart rate through release of a neurotransmitter called noradrenalin.
Parasympathetic impulses cause a decrease in heart rate through the release of a neurotransmitter called acetyl choline.
Hormones such as adrenaline (released during stress from the adrenal medulla) and thyroid hormones from the thyroid gland also accelerate the heart rate.
UHI / CC0
Parasympathetic nerve (inhibitor), pressure receptors in aortic and carotid bodies, chemoreceptors in aortic and carotid bodies, temperature receptors in muscles, stretch receptors in muscles, Sympathetic nerve (accelerator).
Quiz
Blood pressure
Blood pressure is simply a measurement of the pressure exerted by the blood upon the walls of the blood vessels.
This is affected by two things:
The peripheral resistance of the blood vessels
The amount of blood being pumped around the body.
Blood pressure gradually decreases as blood moves away from the heart, through the arteries, through capillaries and into the veins. It is highest in the aorta and lowest in the vena cavae. Normal blood pressure is 120/80mm/Hg. The first or upper reading is that of the systolic pressure, and the second or lower reading is that of the diastolic pressure. The systolic pressure is that in the blood vessels when the ventricles are contracting and the diastolic pressure is when the ventricles are relaxed and filled with blood.
UHI / CC0
(Click image to toggle animation on/off)
Blood vells, heart
Systolic 120mm Hg
Distolic 80 mm Hg
Cardiac output, heart rate and stroke volume
The heart rate (pulse) is how many times the heart beats per minute. Stroke volume is the amount of blood pumped out by the heart with every cardiac contraction. Both of these affect the amount of blood in the circulatory system – this is the cardiac output (CO).
Cardiac output can be calculated as follows:
CO = HR x SV
A higher cardiac output means there will be greater pressure on the blood vessels. Additionally, the diameter of each blood vessel affects the peripheral resistance created by the volume of blood passing through – the smaller the diameter of a blood vessel, the greater the resistance. Therefore, blood pressure increases if a blood vessel is partially or completely blocked, or during vasoconstriction.
UHI / CC0
(Click image to toggle animation on/off)
Blood vells, heart
Systolic 120mm Hg
CO = HR x SV
Controlling blood pressure
The smooth muscle layer in arteries and arterioles contracts (vasoconstriction) and expands (vasodilation) in response to messages from the sympathetic nervous system. An increase in stimulation via the sympathetic nervous system will result in the muscle wall contracting and squeezing together the walls of the artery, narrowing the lumen (artery diameter). This vasoconstriction reduces blood flow to a specific part of the body, and elevates blood pressure.
When blood pressure drops, vasoconstriction in the digestive tract, skin and kidneys reduces arteriole diameter, increasing blood pressure in the major arteries and re-directing blood flow to the heart, lungs, and brain. When blood pressure is too high, a decrease in sympathetic stimulation causes relaxation of the muscles in the artery walls, and the lumen opens up, decreasing blood pressure. As well as helping to control blood pressure, arteries and arterioles vasoconstrict to help limit blood loss from wounds, and vasodilation and vasoconstriction also occur in response to various hormones and to body temperature.
Vasodilation and vasoconstriction
We also vasodilate and vasoconstrict blood vessels to regulate the amount of blood that reaches each part of the body. For example, when digestion is taking place, greater blood flow is required in the digestive system, so blood flow will be increased in that area via vasodilation. When we exercise, we dilate the arterioles in the muscles to provide oxygen and nutrient rich blood for the muscles to use for energy.
Whenever body temperature is high, arterioles near the surface of the skin vasodilate to allow heat to escape via the skin; if body temperature is low, vasoconstriction reduces blood flow at the the surface of the skin which helps to retain heat.
Vasoconstriction and vasodilation may take place in any area of the body where blood flow needs to be reduced or increased.
Blood vessels
Blood is transported through the body by a continuous system of vessels. Blood vessels in the cardiovascular system are:
- Arteries
- Arterioles
- Capillaries
- Venules
- Veins
Arteries transport blood away from the heart under pressure, and veins carry blood back to the heart at a lower pressure.
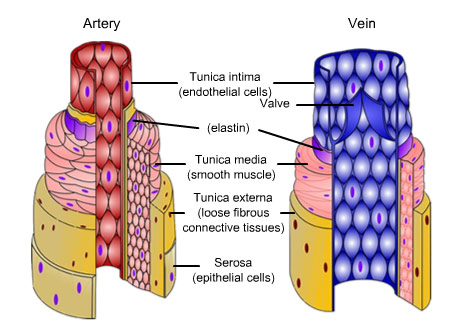
UHI / CC0
Artery
Vein
Tunica intima (endothelia cells)
Valve
Elastin
Tunica media (smooth muscle)
Tunica extrema (loose fibrous connective tissues)
Serosa (epithelia cells)
Arteries and arterioles
Arteries carry blood from the heart to the body tissues. They have thick walls made up of three layers - the innermost layer is an endothelial lining preventing blood from sticking, the middle layer contains elastic tissue and smooth muscle, and the outer layer is a protective coat. The inner channel through which blood flows is called the lumen.
Large arteries such as the aorta, carotid and pulmonary are known as elastic or conducting arteries. These carry blood from the heart to medium sized arteries, and need to accommodate great pressure and blood volume.
Medium-sized arteries are known as muscular arteries; they contain less elastic but more muscle fibres. The walls are thicker and they are capable of greater vasoconstriction and vasodilation than elastic arteries in order to help control the blood flow through the body.
Arterioles are small arteries which control blood flow to the capillaries via vasoconstriction and vasodilation.
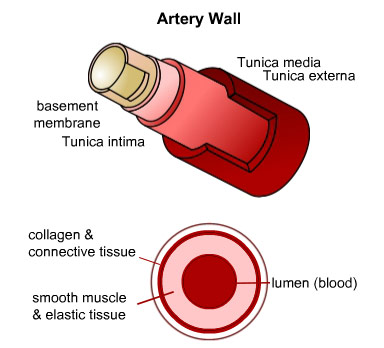
UHI / CC0
Artery wall
Tunica media
Tunica externa
Basement membrane
Tunica intima
Collagen and connective tissue
Smooth muscle and elastic tissue
Lumen (blood)
Capillaries
Capillaries allow exchange of materials between the blood and tissues; capillary walls are one cell thick to allow this exchange. Capillaries are the smallest of the blood vessels, only just wide enough to allow circulation of the blood cells. Blood is oxygenated as it reaches capillaries, but largely deoxygenated as the capillaries join up to form venules.
Capillaries form networks around areas of tissue so that every cell has a blood supply. Tissues with high metabolic activity such as the liver, lungs, kidneys and nervous tissue have higher requirements for nutrients, and therefore have a denser network of capillaries.
UHI / CC0
(Click image to toggle animation on/off)
Artery wall
Arteriole
Venule
Artery
Capillaries
Tissue cells
Vein
Veins and venules
Venules collect waste-rich, de-oxygenated blood from capillaries and drain it into veins, becoming larger as they approach the veins. Veins transport blood back to the heart at a lower pressure than in the arteries.
Veins have three layers similar to those in arteries, but also contain valves which help to keep blood flowing towards the heart and prevent backflow. As veins run through muscles, the contraction of skeletal muscles helps to squeeze blood in the veins back towards the heart as shown in this diagram.
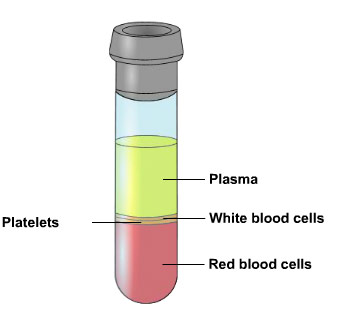
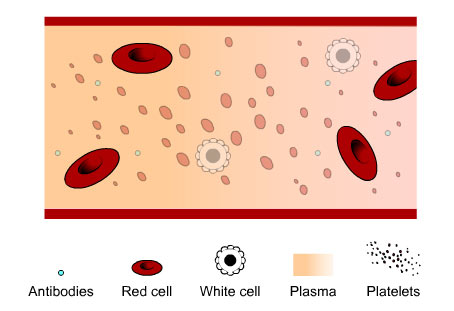
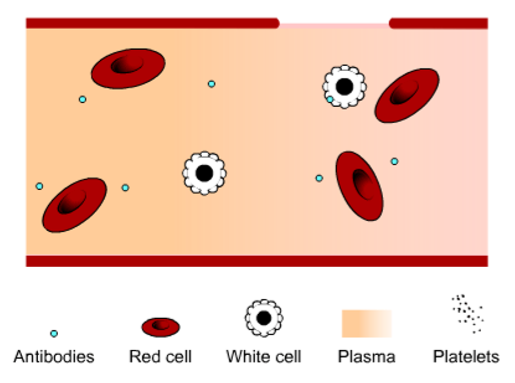
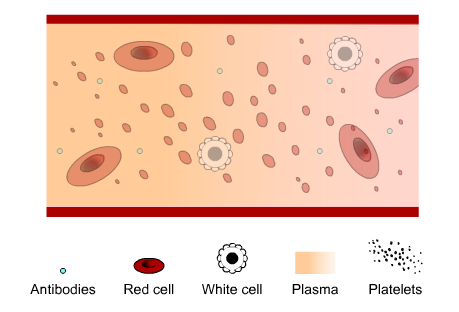
Blood
Blood is a specialized fluid with a pH of approximately 7.4.
Blood is made up of four key components:
- Red blood cells (erythrocytes)
- White blood cells (leukocytes)
- Platelets
- Plasma
It transports substances such as glucose and other nutrients, antibodies, hormones and enzymes around the body. Blood allows transportation of various materials between different cells and tissues of the body, aids in temperature regulation and acid-base (pH) balance, and also aids in protection through immune function.
The functions of blood
Transport of gases
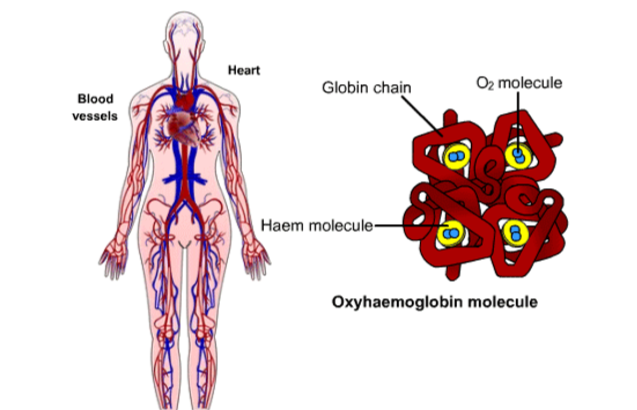
Most oxygen is carried in the blood attached to red blood cells and haemoglobin as oxyhaemoglobin.
A small amount of carbon dioxide (7%) is dissolved in blood plasma, but most is transported as bicarbonate ions (70%) after reacting with water to form carbonic acid and then bicarbonate ions.
The remaining 23% is transported attached to haemoglobin to form carbaminohaemoglobin.
Temperature control
The temperature of blood is maintained at approximately 38°C, slightly higher than normal body temperature of 37°C. Blood picks up heat from the body core or from areas of increased metabolic activity and displaces the heat throughout the body or to the skin when the body is overheated.
pH control
We have a number of mechanisms which enable us to closely maintain an ideal blood pH (acid-base balance) of approximately 7.4. As well as waste products from cells such as lactic acid, carbon dioxide levels in the blood also reduce blood pH and must be constantly monitored and buffered.
Addition of CO2
Removal of CO2
UHI / CC0
Immune function
Blood contains several components that aid immune function. Platelets mesh together at the site of a wound to prevent blood loss and reduce the risk of infection. White blood cells (leukocytes) conduct a number of immune functions within the blood.
UHI / CC0
(Click image to toggle animation on/off)
Blood vessels and blood
Red blood cells - erythrocytes
Erythrocytes are formed in red bone marrow and broken down in the spleen and liver at approximately 2 million every second, the rate of red cell production roughly matching that of destruction.
Red blood cells carry oxygen bound to a protein called haemoglobin, which gives blood its red colour. As blood passes through the lungs, oxygen attaches to haemoglobin forming oxyhaemoglobin.
Erythrocytes have the ability to squeeze through narrow capillaries of a lesser diameter as they have a very flexible cell membrane. However, with no nucleus to resynthesize new cell components to replace damaged ones, they have a cell life of about 120 days.
They have a bi-concave disc shape which increases surface area to maximize oxygen diffusion. Lack of cell organelles increases the space available for haemoglobin and oxygen carriage.
White blood cells - leukocytes
White blood cells (leukocytes) are produced in bone marrow and form part of the immune system, protecting the body from invading microbes.
They are irregularly shaped and have a large nucleus, and there are several types of leukocyte:
- Lymphocytes
- Monocytes
- Neutrophils
- Basophils
- Eosinophils
Some leukocytes make antibodies, some produce anti-toxins that neutralize poisons released by microbes, and have a phagocytic action where they engulf microbes to de-activate them.
Platelets - thrombocytes
Platelets are also formed in bone marrow. They are disc shaped, have no nucleus but contain many granules.
The main function of platelets is to reduce blood loss by forming a platelet plug over any damaged areas in the blood vessel walls.
Their granules also contain chemicals such as fibrinogen, which promote blood clotting when released.
They have a short life span of 5 to 9 days and are removed from the circulation in the liver and spleen.
Plasma
Plasma is the straw coloured liquid component of blood. It makes up 55% of total blood content and consists of approximately 91% water and 8% protein. Plasma transports substances around the body, such as:
- Hormones such as insulin, aldosterone or adrenalin
- Digested products such as amino acids from protein digestion, or glucose from carbohydrate digestion
- Waste products such as urea or lactic acid
- Antibodies
- Blood proteins such as albumin and haemoglobin
- Gases such as oxygen and carbon dioxide
- Vitamins and minerals, and salts such as sodium chloride.
Quiz
Test your knowledge
Here is the embed code
Summary
You have completed your study of the cardiovascular system.
You should now have a good knowledge and understanding of the anatomy and physiology of the cardiovascular system. You should be able to...
- Describe the anatomy of the heart and blood vessels
- Explain the functions of the cardiovascular system
- Describe blood flow through the heart and the body, and know where blood is oxygenated, and where it is de-oxygenated
- Explain the heart beat
- Explain how our heart rate and blood pressure is affected by internal and external factors
- List the different components of blood and their functions in the body.
UHI / CC0