


Introduction
You might work through this system over several weeks, days or hours, but to enhance your learning and enjoyment make sure you break it up into bite-size chunks.
Here are the sections of fluid balance:
As you study Fluid Balance you will learn about:
- Volume and distribution of water in the body
- Body fluids
- Movement of fluids
- Diffusion, osmosis and active transport
- Circulation of interstitial fluid
- Fluid control in the body
Make notes as you study each section, and interact fully with the activities – watch the animations and complete the quizzes.
Take a break at the end of each section – resting your eyes from the computer screen, getting some fresh air or taking a coffee break will improve your ability to focus on your study and take in information.
Give yourself time to think about what you have learned, and time to absorb and understand it.
 UHI / CC0
UHI / CC0
Volume and distribution of fluid in the body
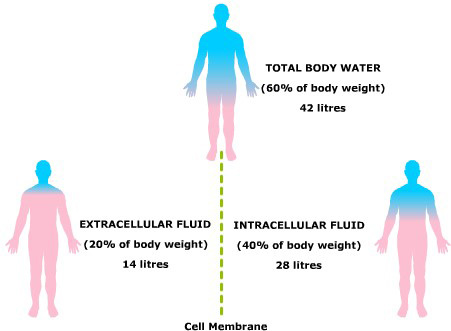
Over half of the human body is made up of water, so it plays a major role in the way the body works. It is needed to transport substances such as nutrients, gases and proteins around the body and in and out of cells, and for chemicals to dissolve into and react with.
The total volume of water in the body under normal conditions depends on age, gender and proportion of body fat. The lower the body mass, the lower the volume of water. Usually men consist of 60% water and women a little less. The proportion of body fat affects the percentage of water content - the higher the body fat percentage, the lower the water content will be.
Note: The fluid % shown in diagram examples is illustrated in blue, and that this shows the % of fluid volume but does not represent where the fluid is in the body.
Water content % is calculated as follows:
% water =
total mass (weight) of waterbody mass
For example, a man who weighs 70kg and has a water volume of 42 litres (1 litre of water = 1kg)
 UHI / CC0
UHI / CC0
Total body water (60% body weight) 42 litres
Extracellular fluid (20% body weight) 14 litres
Intracellular fluid (40% body weight) 28 litres
 UHI / CC0
UHI / CC0
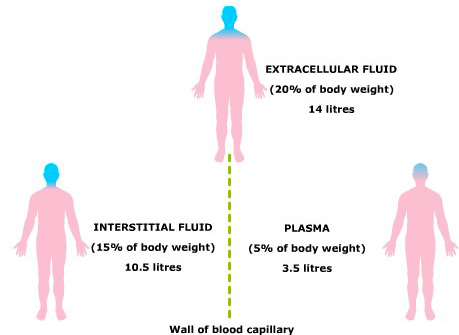
Extracellular fluid (20% body weight) 14 litres
Interstitial fluid (15% body weight) 10.5 litres
Plasma (5% body weight) 3.5 litres
The effect of temperature and exercise on water loss in a normal adult
The body loses and gains water due to normal bodily functions. The way in which the body maintains homeostasis is called water balance.
water loss = water gain
Water can be lost in a variety of essential ways e.g. via the kidneys to remove harmful waste products, via the lungs through breathing, and through sweating when we exercise or in hot weather. Water is lost through the skin at all times but we only become conscious of this when we sweat. Water lost by evaporation through the skin (not sweat) and from the air passages and lungs is called insensible water loss because we are generally unaware of it.
Quiz
Calculate the water % for each of these examples.
| Age (yr) | Mass kg (yr) | Volume water (litres) | % water |
| 0 (newborn) | 4 | 3.0 | |
| 2 | 14 | 9.5 | 68 |
| 7 | 33 | 21.1 | |
| 16 | 58 | 35.4 | |
| 30 | 70 | 42.0 | 60 |
| 80 | 70 | 40.0 |
Body fluids
Fluid is found throughout the body, in blood (plasma), inside cells (intracellular fluid) and outside cells (extracellular fluid), separated by capillary and cell membranes.
The extracellular fluid is separated into plasma (the fluid in blood) and interstitial or tissue fluid (the fluid outside blood vessels). Fluid moves between the plasma and interstitial fluid via the permeable wall of the blood capillary. Another name for interstitial fluid is intercellular fluid as it is the fluid moving between the cells, such as cerebrospinal fluid.
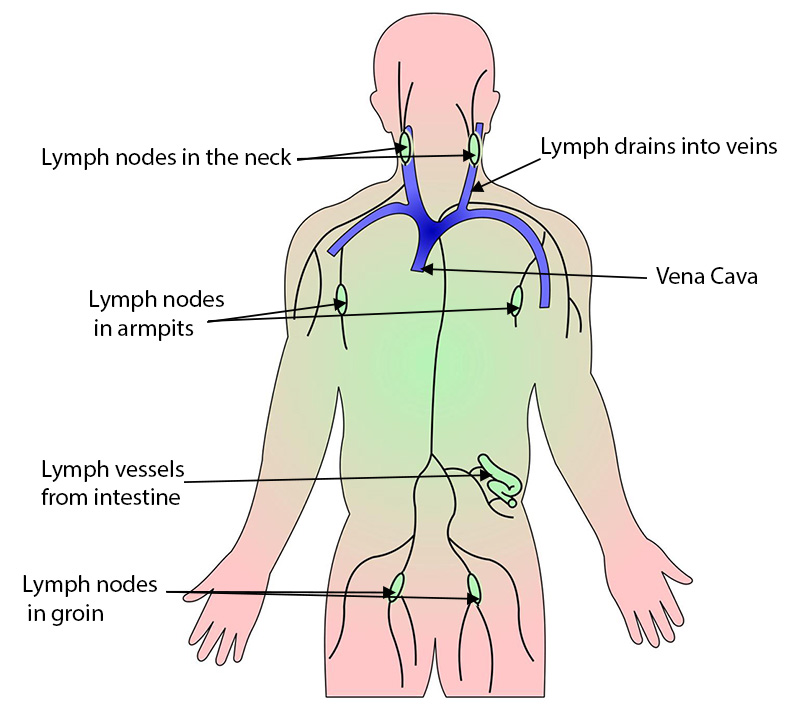
Excess cellular and interstitial fluid drains into lymphatic capillaries through the thin walls, forming lymph.
UHI / CC0
(Click image to toggle animation on/off)
Lymph
Lymph is a milky fluid which is a mixture of interstitial fluid, plasma proteins, toxins and fats. It transports plasma proteins back into the bloodstream and takes away large particles such as bacteria and damaged cells from the tissues where they are filtered as they travel through lymph nodes in the lymphatic system. Filtered lymph is returned to the cardiovascular system via two central (thoracic) lymph ducts, so returning fluid and particles back to the blood.
 UHI / CC0
UHI / CC0
- Lymph nodes in neck
- Lymph drains into veins
- Vena Cava
- Lymph nodes in armpits
- Lymph vessels from intestine
- Lymph nodes in groin
Movement of fluids
Water moves between intracellular (inside the cell) and extracellular (outside the cell) areas through the cell membrane, and between the bloodstream and lymphatic system through capillary walls. Movement of substances across these barriers occurs via diffusion, osmosis and active transport.
UHI / CC0
(Click image to toggle animation on/off)
Blood pressure, plasma, red blood cells, cell of capillary wall, pore, basement membrane, interstitial fluid
Diffusion
Diffusion is the movement of particles across a membrane down a concentration gradient, with substances moving from a region of higher concentration (more particles) to a region of lower concentration (fewer particles).
Both liquids and gases diffuse, but solids do not. Eventually, diffusion causes the number of particles to be evenly spread, and then a solution is then in equilibrium.
If particles gain thermal energy (heat, they move around more and diffuse more readily. Diffusion does not require any energy to occur but will increase if the temperature (and therefore particle movement) increases.
UHI / CC0
(Click image to toggle animation on/off)
Osmosis
If a semi-permeable membrane prevents the movement of particles across the membrane, maybe because they are too large, then instead of particles diffusing across, water may be drawn in the opposite direction instead – this is osmosis.
Osmosis is the diffusion of water across a semi-permeable (selectively permeable) membrane (the membrane selects what moves through the cell membrane). Water is drawn from a high water concentration or potential (low in solutes) to an area of lower water concentration/potential (higher concentration of solutes), and requires no energy.
The presence of a solute (dissolved substance such as salt) decreases the water concentration of a substance - there is more water per unit of volume in a glass of freshwater than there is in an equivalent volume of seawater. In a cell, which has so many organelles and other large molecules, the water flow is generally into the cell.
UHI / CC0
(Click image to toggle animation on/off)
Osmotic balance: hypo and hypertonic solutions
Solutions that are equal in solute concentration are isotonic, and osmosis does not occur. A solution that has a lower solute (solid) concentration than another (and therefore a higher water concentration), is said to be hypotonic to it. A solution that has a higher solute (solid) concentration than another (and therefore a lower water concentration), is said to be hypertonic to it.
For example, distilled water is hypotonic to the cytoplasm in red blood cells, so the blood cells would gain water if immersed in distilled water. Concentrated saline solution (5%) is hypertonic to red blood cell cytoplasm, so water would be drawn out of the cell by osmosis.
Cells placed in hypotonic solutions will gain water; cells placed in hypertonic solutions will lose water; cells placed in isotonic solutions will neither lose nor gain water.
UHI / CC0
(Click image to toggle animation on/off)
UHI / CC0
(Click image to toggle animation on/off)
Osmolarity and osmotic pressure
Osmotic pressure is the pressure that must be applied to a solution to prevent the inward flow of water across a semi-permeable membrane. The more solutes in a solution, the greater the attraction for water to be drawn into that solution.
Consider the following experiment:
Water enters the solution by osmosis and when pressure is applied by the gas cylinder this can slow, stop or reverse osmosis, depending on how much pressure is applied.
The ‘external’ pressure which just balances osmosis, i.e. just keeps water from entering the solution is known as the osmotic pressure of the solution. The greater the concentration of the solution, the greater the pressure needed to prevent osmosis. Thus the osmotic pressure of a solution is proportional to the concentration: high concentration = high osmotic pressure.
Solute-rich solution
UHI / CC0
(Click image to toggle animation on/off)
High pressure needed to prevent water flow in
Lower solute solution
UHI / CC0
(Click image to toggle animation on/off)
Lower pressure needed to prevent water flow in
Isotonic solution
UHI / CC0
(Click image to toggle animation on/off)
Equal pressure - No pressure required to prevent water flow
Circulation of interstitial fluid
If fluid flowed only from the blood into the tissues, the tissues and cells would swell with fluid (oedema) and death would occur. At the arterial end of capillaries the osmotic pressure difference means that water has a natural tendency to enter the capillaries from the interstitial fluid, so the elevated blood pressure inside the capillary at this end is required to push water and solutes out into the interstitial fluid against the osmotic pressure gradient.
To counteract this, much interstitial (intercellular) fluid returns to the blood at the venous end of the capillary beds via osmosis. The high level of proteins in the blood plasma creates an elevated osmotic pressure above that of interstitial fluid, drawing the fluid back in at the venous end of the capillaries. The osmotic pressure of the blood leaving the capillary beds is the same as that entering.
UHI / CC0
(Click image to toggle animation on/off)
Artery, vein, arteriole, precapillary sphincters, venule.
Close up of capillary:
- Fluid squeezed out of capillary by blood pressure
- Fluid reentering capillary by osmotic attraction
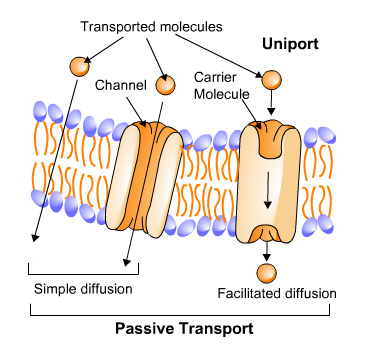
Active/passive transport
Facilitated diffusion and passive transport
Sometimes a carrier molecule known as a transport protein is required to help a particle move across a membrane – this is known as facilitated diffusion.
Passive transport requires no energy from the cell. Examples include the diffusion of oxygen and carbon dioxide, osmosis of water, and facilitated diffusion.
 UHI / CC0
UHI / CC0
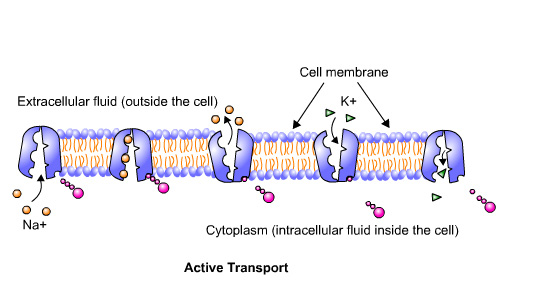
Active transport – the sodium-potassium pump
Active transport moves substances against a concentration gradient from a lower to a higher concentration, which requires the cell to expend energy. One example of this is the sodium-potassium pump.
The cell membrane consists of two layers of phospholipids with two types of protein molecules; one type has channels to allow non-lipid molecules through and the other acts as a carrier molecule. These allow specific substances in and out of cells. Certain molecules like sodium (Na+) and potassium (K+) share the same carrier which is known as the sodium/potassium pump.
The K+ ions are found intracellularly and the Na+ ions are found extracellularly. Both ions want to diffuse down the concentration gradient - K+ wants to move out of the cell and Na+ wants to move into the cell. Homeostasis occurs when excess Na+ is pumped out in exchange for K+, maintaining ionic balance.
 UHI / CC0
UHI / CC0
Quiz
See if you can tell the difference between osmosis, active transport and diffusion.
Fluid control in the body
The body maintains fluid levels at a cellular level through osmotic pressure and the circulation of intercellular fluid. However, water is constantly used in chemical reactions, and lost from the body through sweat, urination, defaecation and respiration, so a constant intake of water is essential.
Homeostasis
Homeostasis is the process which maintains our body’s internal environment within narrow margins. We constantly control:
- Temperature
- blood glucose
- blood pressure
- pH
- water and electrolyte concentration.
Homeostasis is maintained by a dynamic control system which includes:
- detectors (to monitor changes)
- control centres (to process detector information)
- effectors (to return the condition to normal).
 UHI / CC0
UHI / CC0
Regulation of blood volume and blood pressure through Anti- Diuretic Hormone
If we are dehydrated (the body requires more water), we experience the sensation of thirst due to a control centre in the brain creating the desire to drink. However, before this happens the kidneys have already responded to detectors in the body which stimulate a series of events to re-balance water and electrolyte levels.
The kidneys form urine and are therefore closely involved in fluid balance and blood pressure regulation for the whole body. Blood volume and blood pressure are closely controlled through the absorption and secretion of sodium and water in the kidneys under the control of a hormone called anti-diuretic hormone (ADH), also known as vasopressin.
UHI / CC0
(Click image to toggle animation on/off)
Blood water concentration falls > pituitary gland releases more ADH > more water reabsorbed from kidney tubules / small concentration of urine > blood water concentration rises > pituitary gland releases less ADH > less water reabsorbed from kidney tubules / large concentration of dilure urine > and so on...
ADH is secreted from the posterior pituitary in the brain in response to changes in plasma osmolarity (the concentration of solutes in blood). Osmolarity is monitored by brain cells known as osmoreceptors, and these stimulate the secretion of ADH into the bloodstream.
ADH binds to cell receptors in the collecting ducts of the kidney, promoting water reabsorption back into the body. In the absence of ADH the collecting ducts are virtually impermeable to water and it flows out as urine. ADH secretion is also stimulated by decreased blood pressure and blood volume, monitored by baroreceptors in the heart and large arteries, though this is not as sensitive as increased osmolarity. Very high levels of ADH can also cause vasoconstriction to elevate blood pressure.
If blood volume is low (i.e. you are dehydrated), blood pressure may also be decreased and can be elevated by increasing the water volume in the blood.
In response to ADH secretion, water reabsorption back into the body is increased as the walls of the collecting ducts become more permeable to water. Urine is scant and concentrated, blood volume is increased, and blood pressure returns to normal.
If blood volume is high (i.e. you are well hydrated), blood pressure may also be increased and can be reduced by decreasing the water volume in the blood. In response to reduced ADH secretion, water reabsorption back into the body is decreased in the collecting ducts. Urine is plentiful and dilute as more water is passed from the body, blood volume is decreased, and blood pressure returns to normal.
UHI / CC0
(Click image to toggle animation on/off)
Filtrate before it becomes urine.
High water volume / high blood pressure
Less ADH is secreted and water remains in the filtrate making urine dilute and plentiful and reducing water volume in the blood.
Low water volume / low blood pressure
More ADH is secreted and water is reabsorbed back in the body. Urine is concentrated and water volume in the blood is increased.
Quiz
Add the remaining 7 steps into the correct order to illustrate adh regulation. There are 4 answers which are bogus answers.
Can you spot these and leave them out!?
| 1. | Dehydrated |
| 2. | |
| 3. | |
| 4. | |
| 5. | |
| 6. | |
| 7. | |
| 8. |
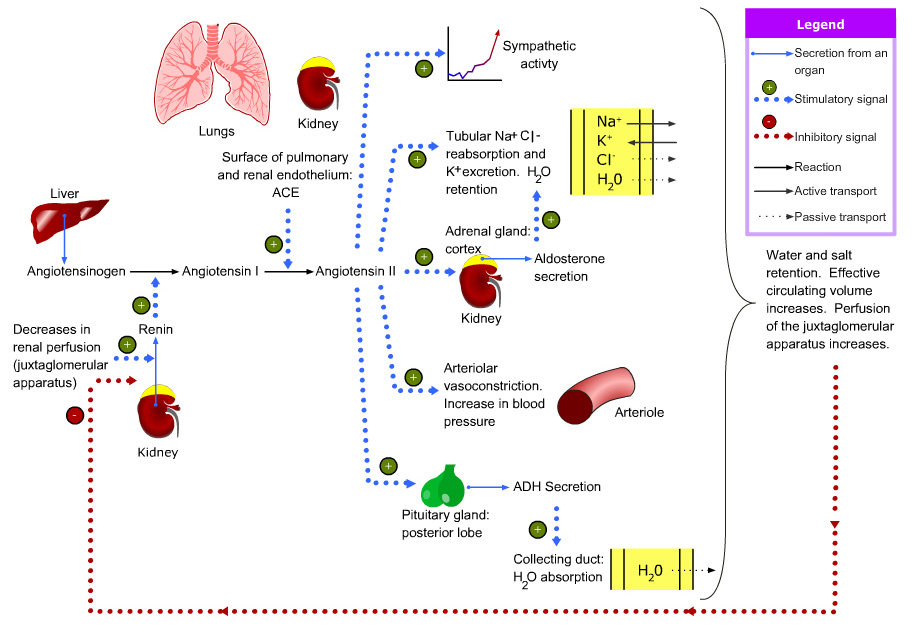
Renin-angiotensin-aldosterone system
Water balance and blood pressure are also controlled through the renin-angiotensin-aldosterone system. When blood volume/blood pressure is low, cells in the afferent arterioles secrete an enzyme called renin, which converts a plasma protein called angiotensinogen (produced by the liver), to be converted to angiotensin 1.
Angiotensin 1 is converted into angiotensin 2 by angiotensin converting enzyme (ACE), formed mainly in the lungs and kidneys. Angiotensin 2:
- is a vasoconstrictor and increases blood pressure
- stimulates aldosterone secretion which increases reabsorption of water and salts, increasing water volume and blood pressure stimulates ADH secretion, increasing water reabsorption and increasing blood pressure.
Renin, angiotensin 2 and high blood potassium all stimulate aldosterone secretion (from the adrenal cortex), which leads to resorption of water and sodium, hence increasing blood volume and ‘switching off’ renin secretion through a negative feedback mechanism.
 UHI / CC0
UHI / CC0
Regulatory action of atrial natriuretic peptide from the heart
There are a number of factors that stimulate the release of atrial natriuretic peptide (ANP) including levels of blood sodium and angiotensin II. However, primary stimulation is atrial stretching in the heart caused by rising blood pressure. Atrial natriuretic peptide (ANP) decreases blood pressure as follows:
- It relaxes arteriole walls resulting in lower peripheral resistance and blood pressure
- It stimulates water and sodium excretion in the kidneys through a number of pathways
- It reduces aldosterone and renin secretion, causing a drop in the reabsorption of water and sodium ions from kidney tubules
This increases urine flow, reduces internal water volume, and decreases blood pressure.
 .jpg?1613574628219)
Test your knowledge
Summary
You have completed your study of fluid balance.
You should now have a good knowledge and understanding of the anatomy and physiology of fluid balance. You should be able to:
- Explain volume and distribution of water in the body
- Explain body fluids
- Explain movement of fluids
- Describe diffusion, osmosis and active transport
- Explain circulation of interstitial fluid
- Explain fluid control in the body
If you think that your knowledge or understanding of any section of the urinary system could be improved further, go back to the relevant sections and work through them again, taking time to make notes and complete the activities.
 UHI / CC0
UHI / CC0