Introduction
You might work through this system over several weeks, days or hours, but to enhance your learning and enjoyment make sure you break it up into bite-size chunks.
Here are the sections of the integumentary system:
The effects of ageing on the skin
The anatomy and function of the nails and hair
As you study the integumentary system you will learn about:
- Anatomy of the Skin
- Functions of the Skin
- The effects of ageing on the skin
- The anatomy and function of the nails and hair
 UHI / CC0
UHI / CC0
Make notes as you study each section, and interact fully with the activities – watch the animations and complete the quizzes.
Take a break at the end of each section– resting your eyes from the computer screen, getting some fresh air or taking a coffee break will improve your ability to focus on your study and take in information.
Give yourself time to think about what you have learned, and time to absorb and understand it.
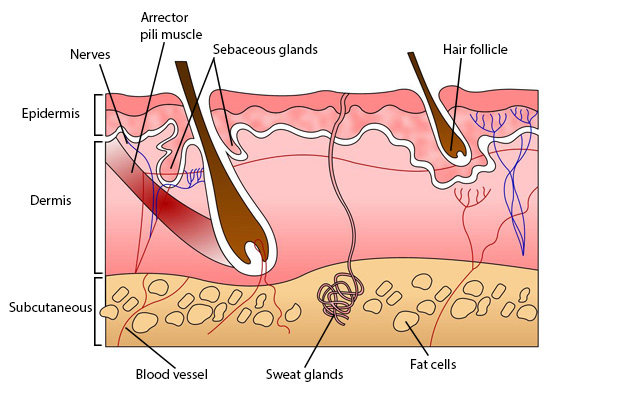
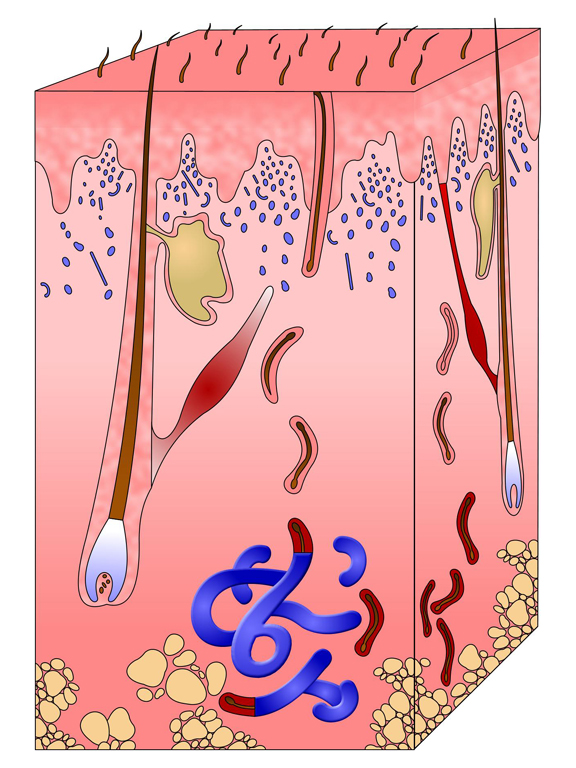
Anatomy of the skin
 UHI/ CC0
UHI/ CC0
- Epidermis
- Dermis
- Nerves
- Arrector pili muscle
- Sebaceous glands
- Hair follicle
- Subcutaneous
- Blood vessels
- Sweat glands
- Fat cells
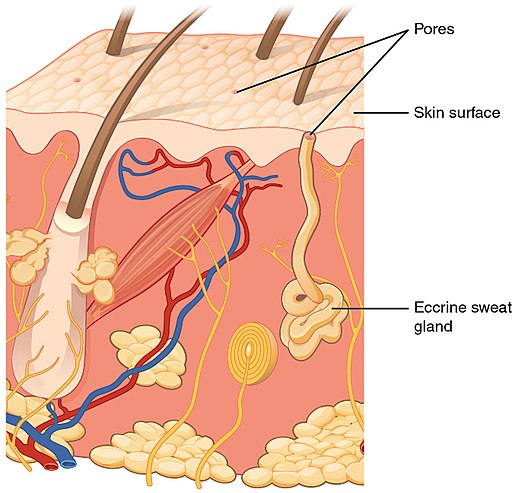
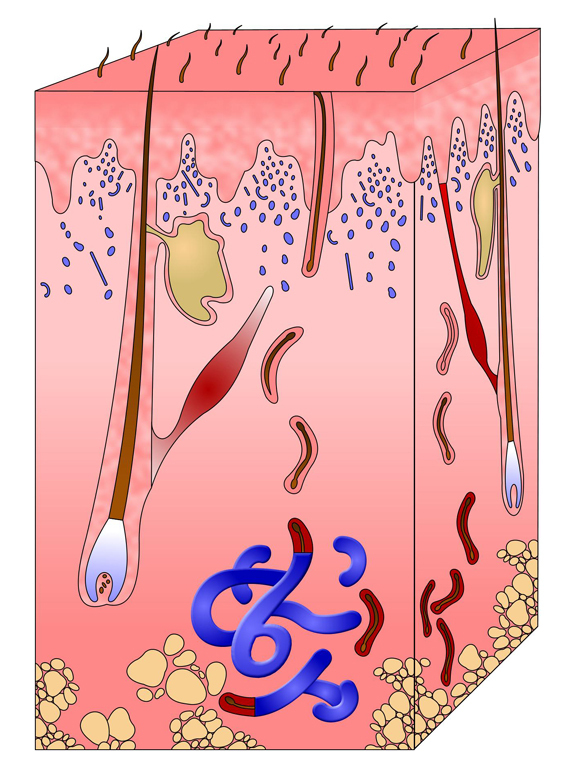
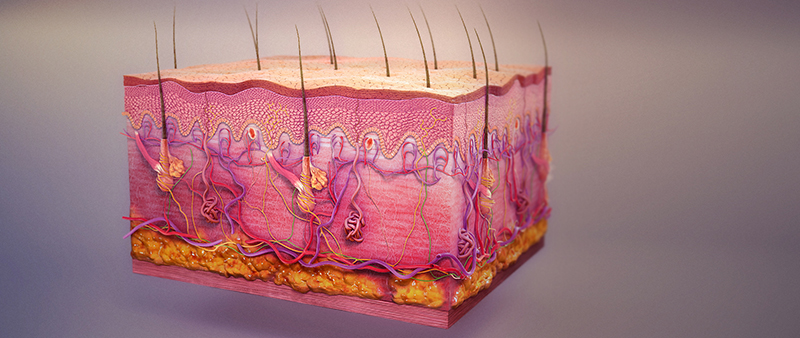
Skin is a type of epithelial tissue which covers the body and is also classed as the largest organ of the body. It contains glands, hair and nails, and is continuous with the mucous membranes which line the body orifices.
The skin has a network of blood vessels which help with regulation of body temperature, and also a network of sensory nerves which enable us to sense and feel temperatures and textures on the skin.
The skin has two main layers:
- the dermis (thicker, connective tissue)
- the epidermis (outer, thinner layer).
Between the skin and underlying structures is a layer of subcutaneous fat which provides insulation and some protection. This is known as the hypodermis or subcutaneous layer.
Epidermis
The epidermis is the most superficial (outer) layer of the skin and is composed of stratified, keratinized squamous epithelium which varies in thickness in different parts of the body (0.05 – 1.5mm), being thickest on the palms of the hands and soles of the feet.
The epidermis contains no blood vessels or nerve endings but has access to nutrients and oxygen from its deeper layers which are bathed in interstitial fluid from the dermis.
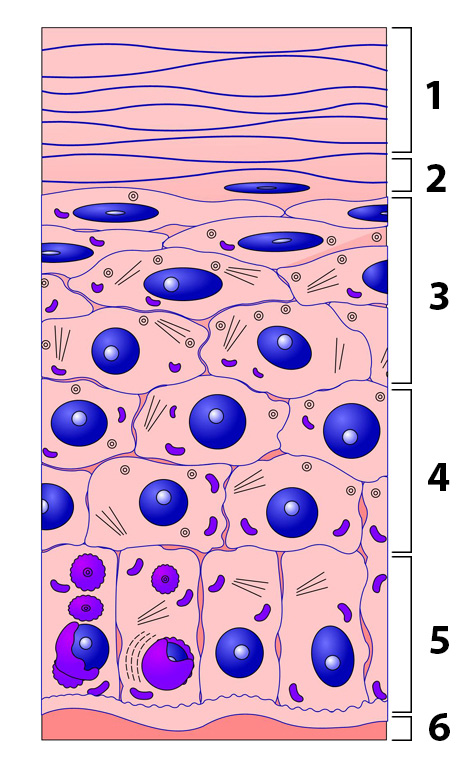
Layers of the epidermis
The cytoplasm of epithelial cells is gradually replaced with keratin as the cells move closer to the skin surface, simultaneously becoming flatter and thinner. The stratum corneum (top layers) are heavily keratinized, particularly the outer horny layer. There are several other layers in the epidermis.
The germinative (basal) layer is where epidermal cells are formed. It is also called stratum basale (basal layer or basal membrane). The stratum spinosum (prickle cell layer) lies above this, then the stratum granulosum (granular layer) divides the
growing cells below from the keratinized, dying cells on the skin surface. The stratum lucidum (clear layer) consists of dead cells packed closely together and is only present in plantar skin on the soles of the feet and palms of the hands.
 UHI/ CC0
UHI/ CC0
- Horny layer
- Clear layer
- Granular layer
- Prickle-cell layer
- Basal layer
- Basal membrane
Epidermal cells
Epidermal cells are formed in the germinative layer and gradually change and become more keratinized as they reach the outer layer of skin. This takes approximately one month and is dependent upon the shedding of the keratinized surface cells, cell keratinisation (adequate but not excessive), and continual cell division.
Hairs, sweat gland ducts and sebaceous secretions all pass through the epidermis to the
surface of the skin. The cells of the outer stratum corneum are dead and constantly sloughed off, being replaced by cells from the layer immediately underneath. The surface of the epidermis is ridged by projections called papillae – this creates the individuality of your fingerprint.
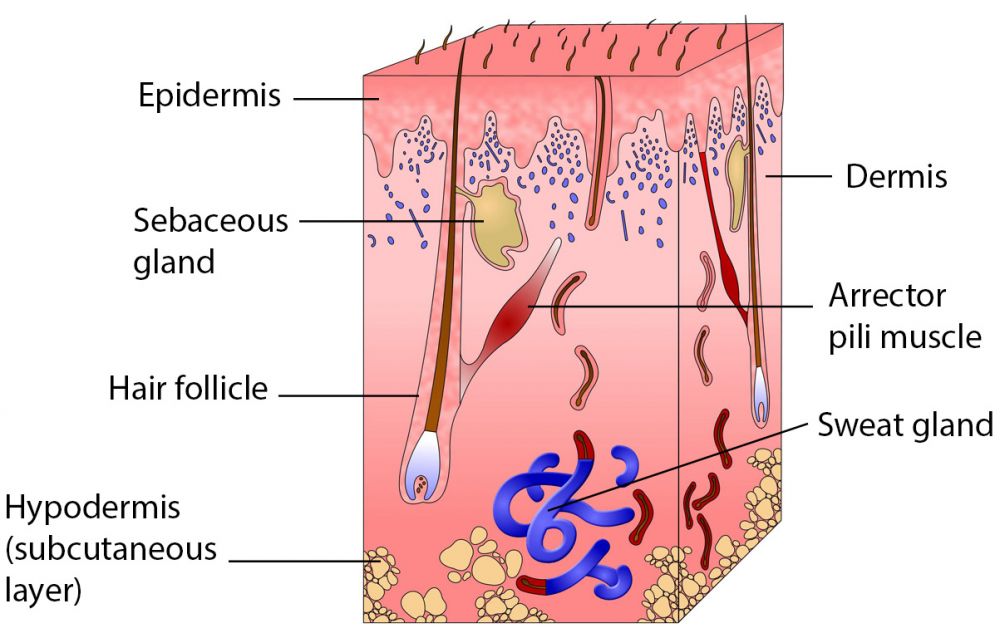 UHI / CC0
UHI / CC0
- Epidermis
- Dermis
- Arrector pili muscle
- Sebaceous glands
- Hair follicle
- Sweat gland
- Hypodermis
(subcutaneous layer)
Dermis
The dermis is tough and elastic and contains collagen which provides strength and elastin fibres creating elasticity. The dermis contains blood and lymph vessels, sensory nerve endings, sweat and sebaceous glands and ducts, hairs and arrector pili muscles.
Fibroblasts, macrophages and mast cells in the dermis provide protection against invading microbes.
The dermis is split into two layers. The deeper reticular layer contains blood vessels, nerves, glands and hair follicles, and the papillary layer which protrudes into the epidermis contains nerve endings and blood capillaries. At the bottom of the dermis is the subcutaneous layer (hypodermis), consisting of adipose tissue and a rich blood supply.
Hair and arrector pili muscles
Hair follicles are lined with cells that synthesize the proteins that form hair. The follicles extend from a cluster of cells called the bulb. Each bulb contains a dermal papilla carrying capillaries and blood supply. Cells in the bulb multiply and are pushed upwards. As they move further from the dermis and receive less nutrition, they die and become more keratinized, forming hairs.
The hair shaft is the part of the hair above the skin surface; hair below the outer epidermis is known as the root. Hard keratin makes up the bulk of the hair shaft, which will not slough off and is more durable and resistant than the soft keratin found in the epidermis.
Arrector pili muscles are small bundles of smooth muscle fibres attached to the hair follicles, stimulated by sympathetic nerve fibres in response to fear and cold. When the muscle contracts the hair is pulled upright, causing a small bump in the skin and allowing the upright hairs to trap a layer of insulating air, hence raising body temperature. This is commonly known as ‘getting goosebumps
The animated diagram below shows that the arrector pili muscle is connected to the hair follicle and the epidermis resulting in the erection of the hair during muscle contraction causing goosebumps.
AnthonyCaccese/ CC BY-SA 4.0
(Click image to toggle animation on/off)
Key
- Epidermis
- Arrector Pili muscle
- Hair follicle
- Dermis
Quiz
Name the areas of skin in the diagram:
Glands
The skin contains different types of glands:
- Sebaceous glands which secrete sebum
- Sweat (sudoriferous) glands which secrete sweat. These are either eccrine or apocrine glands.
Sebaceous glands are found all over the body apart from on the soles of the feet and palms of the hands. They differ in size and are larger on the face, neck and upper chest. They produce sebum which is excreted via the hair follicles. Sebum softens and lubricates the skin, reduces water loss and prevents hair from becoming too brittle, although over-production of sebum causes ‘greasy’ hair and may cause spots or acne if it blocks the hair follicle. It has a bactericidal action in the follicle and on the skin but may cause an infected area if blocking hair ducts. Sebum secretion is stimulated by the production of androgen hormones from the adrenal glands.
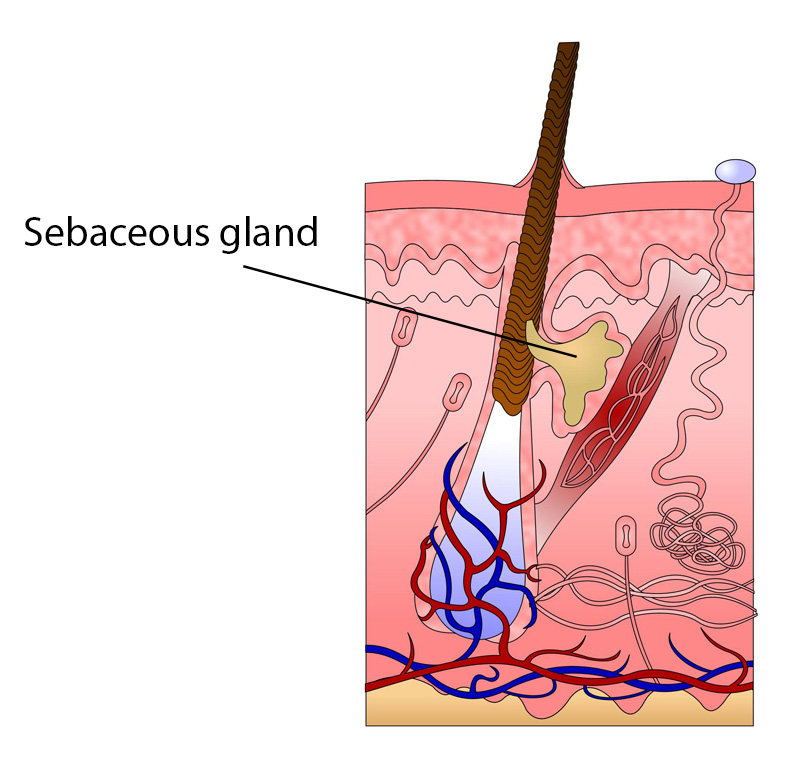 UHI / CC0
UHI / CC0
There are approximately 2.5 million sweat glands all over the body, with the exception of the lips, parts of the external genitalia and nipples. Sweat glands are a blind-ended coiled tube in the dermis, extending through the epidermis and opening out into hair follicles or tiny depressions in the skin called pores.
Apocrine glands are found in the axillary and anogenital areas and do not become active until puberty. They are larger than eccrine glands and their ducts open into hair follicles. The composition of the sweat excreted by these glands is similar to that excreted by the eccrine glands but also contains fatty materials and proteins which can give sweat a milky appearance. Although sweat itself has no discernable scent, odours may arise as it is broken down by bacteria on the skin surface.
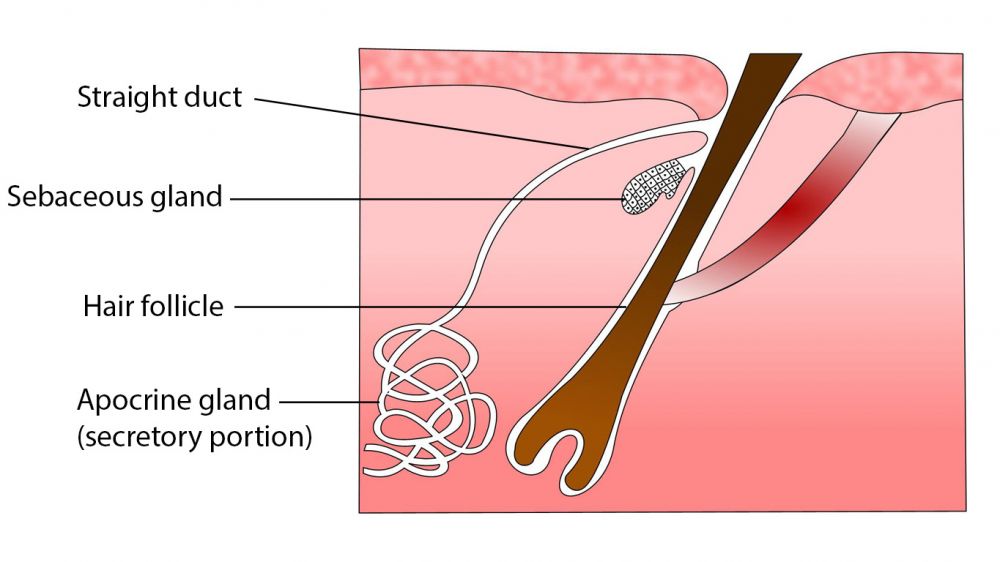 UHI / CC0
UHI / CC0
Straight duct, sebaceous gland, hair follicle, apocrine gland (secretory portion)
Eccrine glands are more abundant and many are located in the plantar skin on the palms of the hands and soles of the feet. Each eccrine gland is a coiled tube with a blind end in the dermis and a duct extending out onto the skin surface.
Sweat glands are surrounded by a dense network of capillaries. Sweat is mostly comprised of water derived from blood plasma. It also contains waste products such as urea and lactic acid from the cardiovascular and lymphatic systems. It is acidic with a pH of between 4 – 6, which helps to reduce pathogenic bacteria and fungal infections on the skin. Sweat composition is affected by genetics and through diet.
Pores, skin surface with opening of eccrine gland, eccrine gland below surface
Quiz
Put the options below to the correct gland.
Functions of the skin
The key functions of the skin are as follows:
- It provides a protective layer and a range of defence mechanisms against physical amage, microbes and infections.
- It prevents loss of extracellular fluid It contains sensory nerve endings enabling us to sense temperature, textures and pain.
- It is involved in the regulation of body temperature.
- It is able to absorb some substances and excrete toxins.
- It produces Vitamin D and melanin.
 scientific animations/ CC BY-SA 4.0
scientific animations/ CC BY-SA 4.0
Defence mechanisms
The skin has a range of defence mechanisms:
- Nerve endings provide information that keeps us away from hot and rough surfaces that could burn or penetrate the skin.
- The acidic pH created by the secretion of sweat and sebum helps to prevent the multiplication of bacteria and fungi, and keratinized skin forms a continuous barrier which prevents entry of toxic substances and microbes into the body.
- The skin also contains macrophages and Langerhans cells in the epidermis which form part of our immune response, and are able to recognise and phagocytose foreign matter which may have entered the skin.
When a microbe penetrates the skin, or when the skin surface is cut, the inflammatory response occurs, resulting in inflammation, redness, heat and pain.
Absorption and excretion
Although the skin provides a protective and waterproof barrier, some substances can penetrate the epidermis, such as oxygen and carbon dioxide, and lipid soluble substances like steroids (as in steroid creams) and fat soluble vitamins (A, D, E and K). For, example, contraceptive medications and nicotine patches administer drugs through the skin.
The skin also secretes sweat and sebum, which create an acidic pH with anti-microbial properties. Sweat aids in temperature regulation and also carries out toxins such as urea and lactic acid, whilst sebum contributes to the condition of skin and hair.
Temperature regulation through vasodilation and vasoconstriction
The skin is a key factor in temperature control as heat losses occur mainly from the body surface through the skin. As well as the insulating subcutaneous fat layer beneath the dermis minimising heat loss through the skin, body temperature is controlled by a group of temperature sensitive nerve cells in the skin which feed information to the hypothalamus in the brain.
Most of the heat arriving at the body surface is carried by the blood, and blood flow control to the superficial capillaries in the skin is a very effective way of regulating body temperature. After sensing a change in body temperature in the skin, a nervous impulse is sent to the involuntary muscle in the walls of the arterioles feeding the superficial skin capillaries. Through dilating (opening) or constricting (closing) these arterioles we are able to control our body temperature.
With vasodilation and increased capillary blood flow in the skin, heat can be transferred from the body to the outside. Heat loss in water is greater, so during profuse sweating or when swimming heat loss is further enhanced. If heat loss is not sufficiently rapid, the sympathetic nervous system stimulates sweat glands to increase sweat production.
Sweating enables heat loss through the evaporation of water on the skin, as water absorbs heat energy when it turns into water vapour. At high temperatures or during exercise, the accelerated sweating provides a larger volume of water to enhance the evaporative cooling effect. Air currents also accelerate evaporation and enhance the cooling effect.
At low external temperatures our arterioles vasoconstrict to reduce blood flow to the skin and limit heat loss.
Vasodilation
UHI / CC0
(Click image to toggle animation on/off)
If the arterioles are vasodilated, blood flow to the skin is increased and the skin appears pink or red.
Vasoconstriction
UHI / CC0
(Click image to toggle animation on/off)
If the arterioles are vasoconstricted, blood flow to the skin is reduced and the skin appears pale, even blueish in colour.
Sensory reception
The skin contains sensory receptors and corpuscles which monitor pain, pressure (touch) and temperature. Sensory receptors in the epidermis of the fingers and lips make these areas very sensitive to touch.
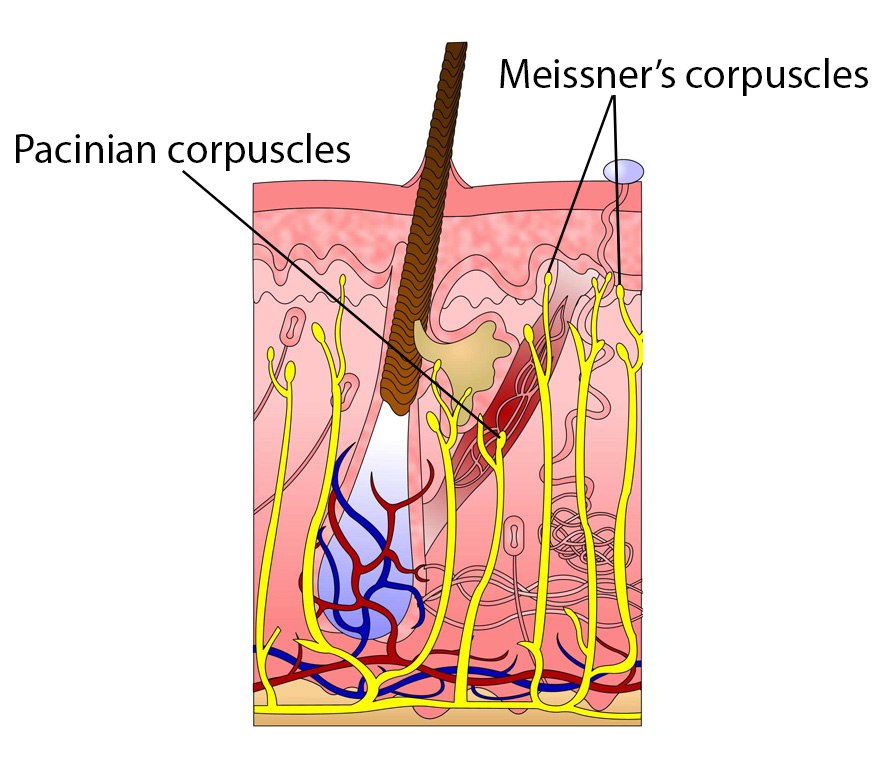 UHI / CC0
UHI / CC0
Production of vitamin D and melanin
Cells called melanocytes in the basal layer of the epidermis synthesize melanin, a pigment which provides some protection against ultraviolet radiation and gives the skin its colour. Skin colour is caused mainly by the number and distribution of melanocytes, with darker skin producing more melanin.
The skin also assists in the synthesis of vitamin D. When the skin is exposed to ultraviolet light (sunlight), a lipid-based substance in the skin called 7-dehydrocholesterol is converted into vitamin D (cholecalciferol).
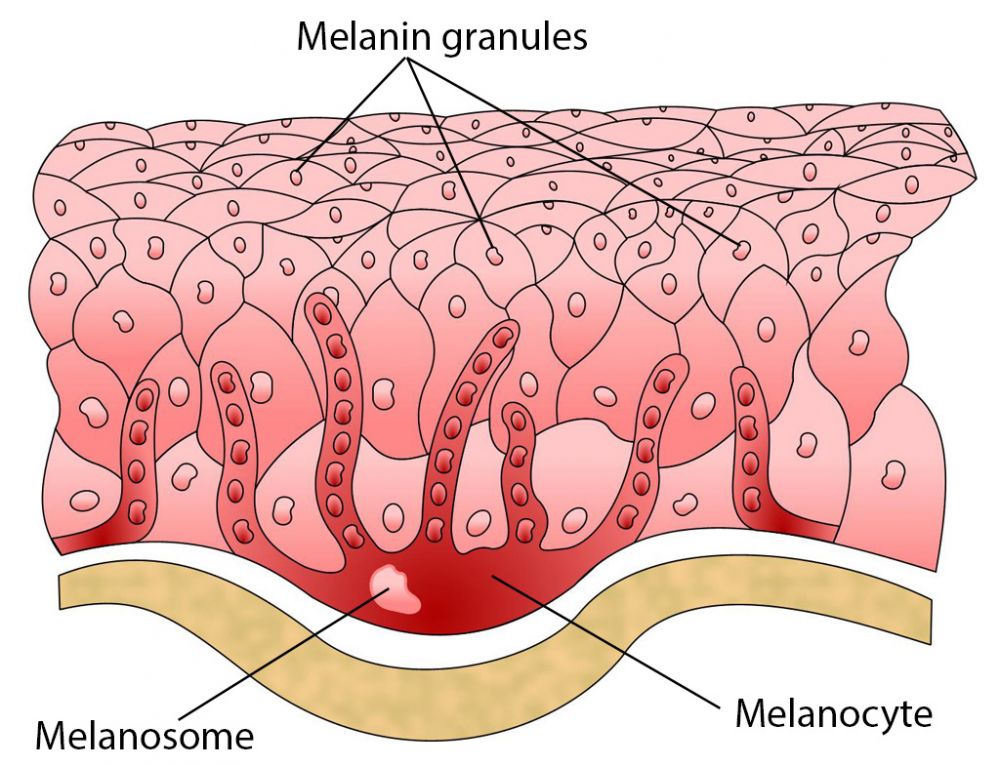 UHI / CC0
UHI / CC0
Quiz
Answer the following questions. There are 8 questions to answer.
Ageing of the skin
A number of mechanisms contribute to the symptoms associated with older skin, such as wrinkles, sagging skin and uneven skin tone.
Fibroblasts (which produce elastin and collagen fibres) reduce in number, so levels of collagen and elastin fibres decrease. With less collagen and elastin fibres, the skin loses some of its elasticity and skin tone (tightness) and can begin to sag. The collagen and elastin fibres can also break, creating wrinkles.
Reduced skin turnover results in dead skin cells remaining on the outer epidermal layer for longer, affecting the appearance of the skin, and reduced sebaceous secretion results in drier skin. These effects plus less subcutaneous fat accentuates the appearance of wrinkles.
Fewer melanocytes (which secrete melanin) results in grey hair and different skin pigmentation including pigmented areas known as liver spots.
Skin damage
 ©BYU
©BYU
As immune defences in the skin become less effective the skin is more susceptible to the effects of microbes and toxins. Digestive processes are also often detrimentally affected with age, providing fewer nutrients for good skin health.
Anti-oxidants such as beta carotene, vitamin E and zinc can all help to reduce free radical damage to cells and reduce some of the effects of ageing, but if absorption of these nutrients from the diet is poor, less nutrient support is available for immune function in the skin and for cell repair and renewal.
The ultraviolet (UVA and UVB) rays in sunlight cause photo-damage of the DNA (deoxyribonucleic acid) in epidermal cells and in collagen and elastin in the dermis. Cell renewal is affected and skin ageing is accelerated by repeated sun exposure.
The anatomy and function of the nails and hair
Nails
The nails are a modified form of the epidermis and are designed to protect the ends of the fingers and toes. Each nail has a free edge, a body and a root which is embedded in the skin. The skin around the nail folds over the proximal and lateral edges of the nail for protection. The fold of skin at the bottom (proximal edge) of the nail is called the eponychium or cuticle.
The epidermal cells forming the nail lie beneath the nail as the nail bed. The nail matrix is responsible for nail growth. It is covered by a white crescent called the lunula. As cells are produced by the nail matrix they become heavily keratinized and grow over the nail bed.
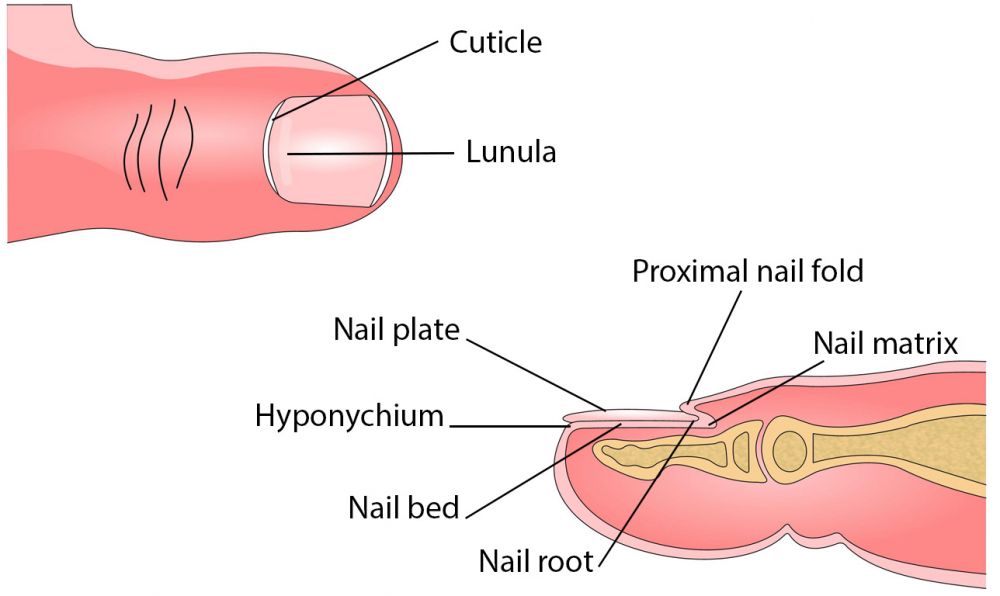 UHI / CC0
UHI / CC0
Cuticle, lunula, proximal nail fold, nail plate, nail matrix, hyponychium, nail bed, nail root.
Hair
Video
Structure of hair follicle - hair color - how does hair growth work (YouTube 2:49)
Test your knowledge
Now it's time to test your knowledge of the integumentary system.
You might want to take some time to read your notes or draw diagrams before you test yourself!
Summary
You have completed your study of the integumentary system.
You should now have a good knowledge and understanding of the anatomy and physiology of the integumentary system. You should be able to:
- Identify and name the major parts of the skin
- Explain the functions of the skin
- Discuss the effects of ageing on the skin
- Describe the anatomy and physiology of hair and nails
If you think that your knowledge or understanding of any section of the integumentary system could be improved further, go back to the relevant sections and work through them again, taking time to make notes and complete the activities.
 UHI / CC0
UHI / CC0