Introduction
You might work through this system over several weeks, days or hours, but to enhance your learning and enjoyment make sure you break it up into bite-size chunks.
Here are the sections of the lymphatic system:
As you study the lymphatic system you will learn about:
- Organisation of the lymphatic system
- Lymph
- Anatomy of the lymphatic system
- Organs of the lymphatic system
- Functions of the lymphatic system
- Immune function
Make notes as you study each section and interact fully with the activities – watch the animations and complete the quizzes.
Take a break at the end of each section– resting your eyes from the computer screen, getting some fresh air or taking a coffee break will improve your ability to focus on your study and take in information.
Give yourself time to think about what you have learned, and time to absorb and understand it.
You can use the notes area and save to your computer at any point during your study.
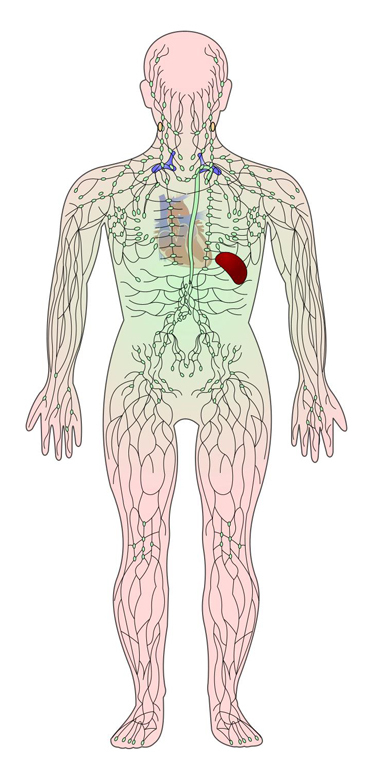
UHI / CC0
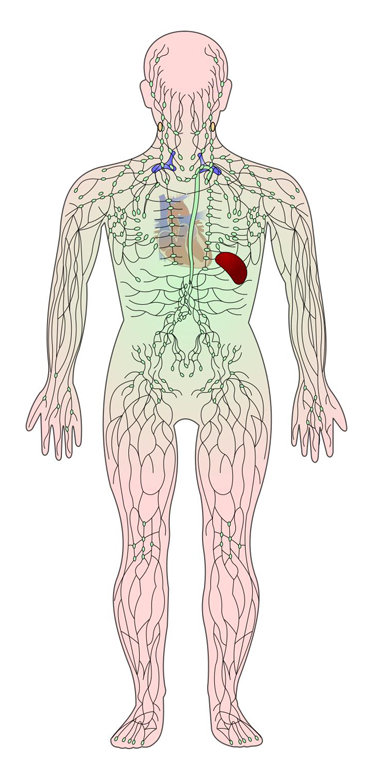
The lymphatic system
The lymphatic system consists of a network of lymph vessels and dense areas of lymphoid tissue, some of which form lymphatic organs.
Functions of the lymphatic system are:
- transportation of dietary fats and fat soluble vitamins A, D, E and K
- draining excess interstitial fluid from tissues to avoid oedema (swelling)
- carrying out immune responses.
It performs all of these tasks through a fluid called lymph. Any cellular waste which does not diffuse back into the bloodstream enters the lymphatic system. Lymph is made up of diffusible fluids from the blood and cells of the body, such as waste products, digested fats, water and some blood proteins.
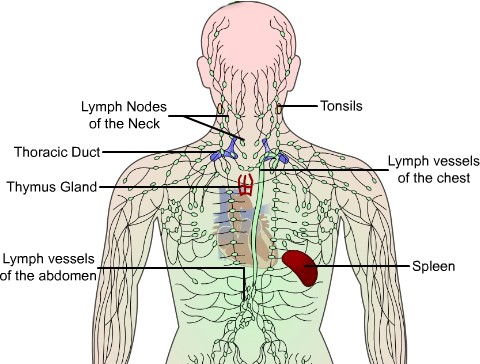
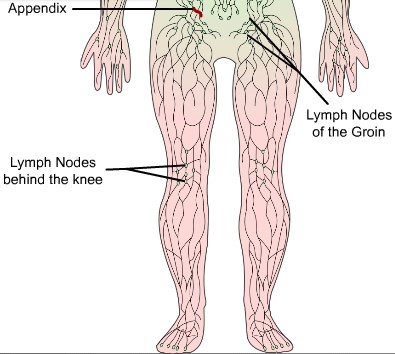
UHI / CC0
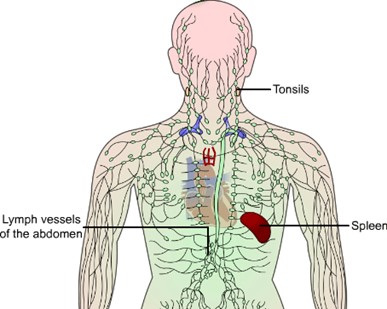
- Lymph nodes of the neck
- Tonsils
- Thoracic duct
- Lymph vessels of the chest
- Thymus gland
- Lymph vessels of the abdomen
- Spleen
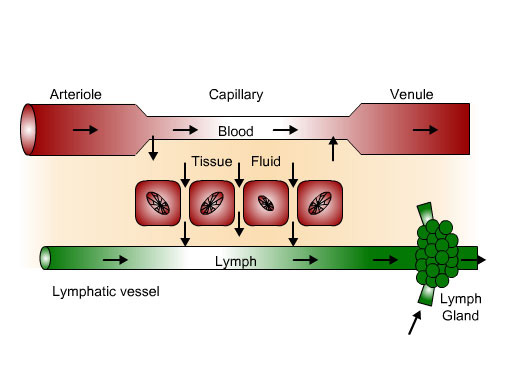
Most components of blood plasma (the straw-coloured, fluid component of blood) filter through the capillary walls to form interstitial fluid in between the cells of the body. This fluid contains substances which are diffusing into or out of cells such as waste products. Some of this fluid carrying cellular waste products diffuses into lymphatic vessels forming lymph.
Lymph is a milky fluid made up of lymphocytes, proteins and fats. It travels around the lymphatic system and empties back into the bloodstream. By having access to the circulation, the body is able to eliminate products of cellular breakdown and bacterial invasion.
Lymphatic capillaries and vessels are present wherever there are blood vessels to allow the major constituents of plasma, interstitial fluid and lymph to move between the bloodstream, lymphatic system and intercellular fluid (interstitial fluid).
Large blood proteins that cannot diffuse out of blood capillaries remain in the blood, making plasma more protein-rich than interstitial fluid or lymph. Plasma proteins that are small enough to pass into the lymph system are returned to the bloodstream when lymphatic fluid empties back into the bloodstream.
Blood plasma, interstitial fluid and lymphatic fluid are similar, but are found in different locations:
- Plasma is found within the blood vessels
- Interstitial fluid is found surrounding the cells and tissues
- Lymphatic fluid is found in lymphatic capillaries and lymphatic vessels.
Organisation of the lymphatic system
The lymphatic system consists of a network of vessels called lymphatic vessels, organs and structures containing lymphatic tissue and lymph. Blood cells called lymphocytes are formed in red bone marrow, so this part of the bone also constitutes a part of the lymphatic system.
The lymphatic system is made up of:
- lymph
- lymphatic capillaries
- lymphatic vessels
- lymphatic trunks
- lymphatic ducts
- lymph nodes lymph organs (spleen and thymus)
- lymphoid tissue (the tonsils, appendix, bone marrow, and Peyer‟s patches in the small intestine)
See diagram on the previous page
Lymphatic capillaries and lymphatic vessels
Lymph vessels begin as lymphatic capillaries which are closed at one end and located in between cells. The capillaries join to create lymphatic vessels, which are similar to veins but have thinner walls and more valves. The valves ensure the one-way flow of lymph around the body. Plasma passes from blood capillaries into the tissues and then enters the lymphatic system through small openings in the lymphatic capillaries.
In the skin, lymphatic capillaries follow veins; in the internal organs, they follow arteries. Areas without lymphatic capillaries include the central nervous system, bone marrow and parts of the spleen and those areas without a good blood supply, such as cartilage, the epidermis and the cornea of the eye.
UHI / CC0
(Click image to toggle animation on/off)
The journey of lymph flow around the body
As well as the valves in the lymphatic vessels, skeletal muscle contractions and internal pressure changes through respiration also aid in maintaining lymph flow around the body.
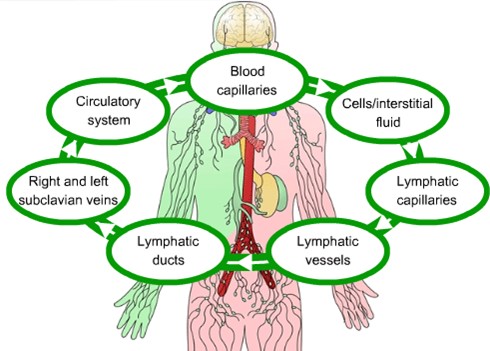
UHI / CC0
Blood capillaries > cells/ interstitial fluid > lymphatic capillaries > lymphatic vessels > lymphatic ducts > right and left subclavian veins > circulatory system > blood capillaries...
Quiz
Click on each term and drag it to its appropriate location. If you are incorrect, the term will return to it's original location.
Lymphatic ducts
Lymphatic vessels join up to form lymphatic trunks (ducts). The right lymphatic duct drains lymph fluid from the upper right quarter of the body above the diaphragm into the right subclavian vein. The thoracic duct in the pleural cavity drains lymph from the rest of the body into the left subclavian vein.
Lymph nodes
As lymph flows through the lymphatic vessels, it flows through lymph nodes. These form approximately 600 tiny, oval structures in the lymphatic system and are located mainly in the neck, groin and armpits, but are also scattered along the lymph vessels. Lymph nodes produce lymphocytes, formed from encapsulated masses of B cells and T cells, creating lymphatic tissue. The B and T cells act as barriers to infection by filtering out and destroying toxins and germs.
Lymph nodes are divided into the inner and outer cortex. The outer cortex contains groups of B cells called lymphatic nodules. The inner cortex does not contain lymphatic nodules but consists mainly of T cells.
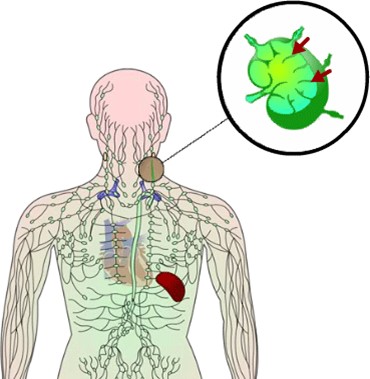
UHI /CC0
Lymph nodules
Lymphatic nodules are areas of lymphatic tissue which are not encapsulated. They are scattered throughout the connective tissue of membranes lining the gastrointestinal, urinary, respiratory and reproductive tracts; areas within the human body most closely associated with the external environment require this additional immune function.
Large masses of lymphatic nodules occur along the gastrointestinal tract at the tonsils, appendix and Peyer‟s patches in the small intestine. The lymphatic tissue in these areas is positioned to provide immune responses to inhaled or ingested substances which may be harmful.
Quiz
Click on each term and drag it to its appropriate location. If you are incorrect, the term will return to it's original location.
Other areas of lymphatic tissue
Lymphatic tissues are areas of dense lymphoid tissue and are one of two types.
Primary lymphatic tissues – stem cells divide and become immuno-competent, and able to mount an immune response. This includes red bone marrow and the thymus.
Secondary lymphatic tissues – these are where most immune responses occur and this includes the spleen, lymph nodes (those not situated along lymphatic vessels) and lymphatic nodules (located in large numbers in the tonsils, Peyer‟s patches and appendix).
Development of secondary lymphatic tissues
Red bone marrow contains stem cells which divide and differentiate (grow) into lymphocytes. Many of the lymphocytes then migrate naturally to the secondary lymphoid tissues where most immune responses occur.
Lymphocytes which pass directly from bone marrow to secondary lymphoid tissues are called B lymphocytes (B cells). Some lymphocytes migrate to the thymus gland and complete a maturation process there before migrating to the secondary lymphoid tissues. These are called T lymphocytes (T cells). A number of additional white blood cells (leukocytes) are also produced in the bone marrow, all with immune functions.
Organs of the lymphatic system
The thymus
The thymus gland is situated between the sternum and the aorta. It is large in infants but after puberty, adipose and connective tissue replace much of the thymic tissue, and by adulthood, the gland is much smaller. Before it reduces in size, it populates the secondary lymphatic organs and tissues with T cells. Some T cells continue to proliferate in the thymus gland throughout life.
The thymus has two lobes, each encapsulated in and held together by connective tissue. Extensions of the capsule called trabeculae extend into the lobes, dividing the lobes into lobules. The outer cortex of each thymus lobule contains a large number of T cells, dendritic cells and macrophages. Immature T cells migrate from red bone marrow to the thymus gland where they proliferate and mature. Dendritic cells in areas such as lymph nodes play a key role in immune function. The medulla contains more mature T cells, dendritic cells and macrophages.
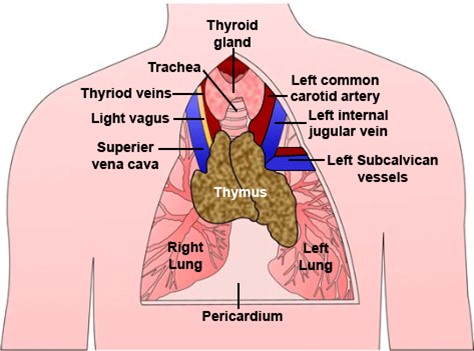
UHI /CC0
- Thyroid gland
- Trachea
- Thyroid veins
- Left common carotid artery
- Left internal jugular vein
- Light vagus
- Superior vena cava
- Left subcalvican vessels
- Thymus
- Right lung
- Left lung
- Pericardium
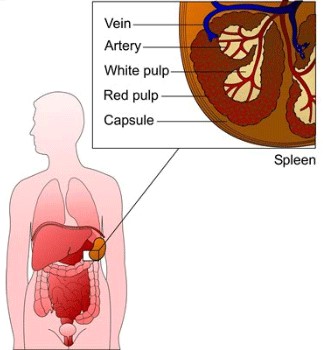
The spleen
The spleen is located between the stomach and diaphragm on the left-hand side of the body and is the largest single area of lymphatic tissue. It is a reservoir for blood and filters the blood and lymph fluid that flows through it. It consists of two types of tissue called white pulp and red pulp.
White pulp is lymphatic tissue consisting of lymphocytes and macrophages arranged around a central splenic artery. As blood flows through the spleen, B and T cells in the white pulp carry out immune functions and macrophages destroy pathogens in the blood through phagocytosis.
The red pulp is arranged around the venous blood supply and consists of blood-filled venous sinuses and cords of tissue called splenic cords. The cords consist of red blood cells, macrophages, lymphocytes, granulocytes and plasma cells. Red pulp removes worn out or damaged red blood cells and platelets, stores platelets, and produces blood cells (haemopoiesis) during foetal development.
Functions of the lymphatic system
Functions of the lymphatic system are:
- Transportation of dietary fats and fat soluble vitamins A, D, E, K
- Draining excess interstitial fluid from tissues to avoid oedema and help manage water balance in the body
- Carrying out immune responses.
In the following pages, you will learn more about each of these functions.
 UHI /CC0
UHI /CC0
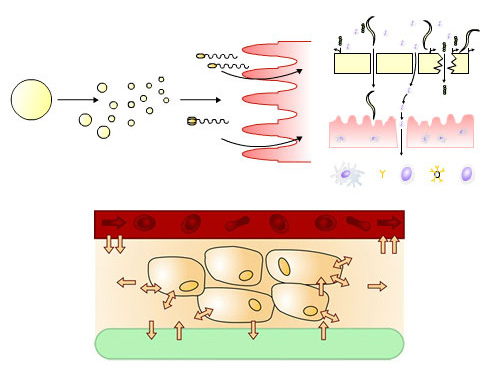
Transport of fats around the body
Most nutrients are absorbed directly into the bloodstream from the digestive tract, but the majority of dietary fats such as those found in butter, oils, meats, fish, eggs and dairy produce are broken down in the digestive system into triglycerides, then enter the lymphatic system.
Triglycerides are then broken down into glycerol or a mono-glyceride molecule (glycerol with one fatty acid chain still attached) and free fatty acid chains, pass through the intestinal wall into the lymphatic system via lacteals, first re-forming into triglycerides and attaching to protein molecules to form chylomicrons, creating a milky fluid called chyle as they mix with the lymph fluid. Fats are then transported in lymph from the small intestine to the bloodstream, emptying into the left subclavian vein and travelling on to the liver.
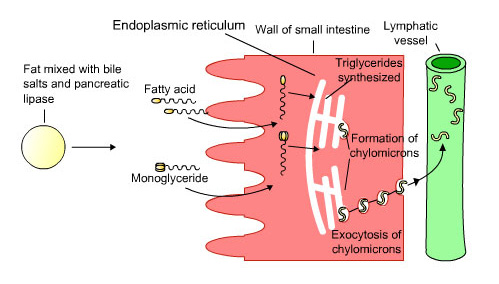 UHI / CC0
UHI / CC0
Fat mixed with bile salts and pancreatic lipase > fatty acid and monoglyceride pass through the wall of small intestine > endoplasmic reticulum: Triglycerides synthesized, formation of chylomicrons, exocytosis of chylomicrons > Lymphatic vessel
Fluid control and prevention of oedema
Most components of blood plasma flow freely out of the capillaries and form interstitial fluid. The fluid that is not reabsorbed into the capillaries - approximately 3 litres per day - drains into the lymphatic system to become lymph, which helps to prevent water retention (oedema) in and around the tissue cells.
UHI / CC0
(Click image to toggle animation on/off)
Immune function
It is largely through the lymphatic system that our body is able to fight infection and ward off invasion from foreign bodies.
The lymphatic system carries out immunological functions in several ways:
- it filters out organisms that cause disease
- it produces white blood cells
- it generates antibodies
We are surrounded by potentially harmful micro-organisms (microbes) such as bacteria, viruses and fungi at all times. These microbes may land on our skin, or enter our body from the air we breathe and from our food. The skin and the epithelial lining (mucous membranes) of our lungs and gastrointestinal tract are physical barriers which prevent many of these microbes from entering our tissue fluids and blood, forming the first line of defence.
 UHI / CC0
UHI / CC0
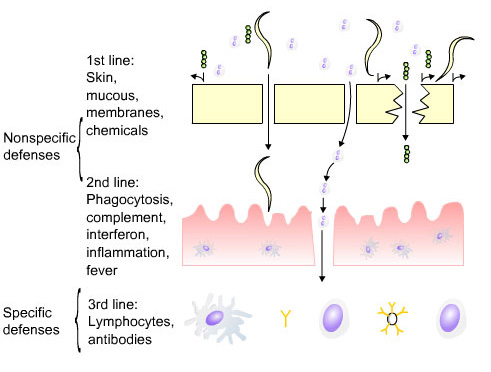
Non-specific defences:
- 1st line - skin, mucous membranes, chemicals
- 2nd line - phagocytosis, complement, interferon, inflammation, fever
Specific defences:
- 3rd line - Lymphocytes, antibodies
Innate immunity
Disease occurs when micro-organisms invade epithelial surfaces and cause infection. Considering our constant exposure to micro-organisms it is surprising that we enjoy long infection-free periods, and that infection is the exception rather than the norm. This resistance (immunity) which prevents entry of micro-organisms into tissues or, once they have gained entry, eliminates them prior to the occurrence of disease, is a characteristic which is present from birth, and therefore, called innate (natural) immunity.
Innate immunity:
- is present from birth
- is non-specific, acting on many organisms rather than specific ones
- does not become more efficient on subsequent exposure to the same organisms
First line defences of the immune system
First line defences are innate (present from birth), non-specific defences as they apply to the majority of microbes and foreign bodies. Physical barriers and mechanisms include:
- Skin
- Mucous membranes
- Nasal hairs
- Prevention of stasis: peristalsis in the gut, urine flow, and cilia (small hairs) move secretions upwards in the bronchial tree.
Also, chemical secretions play an important role in destroying or inhibiting the growth of micro-organisms:
- Tears
- Saliva
- Mucus
- Stomach acid and bile
- Urine
- Vaginal secretions
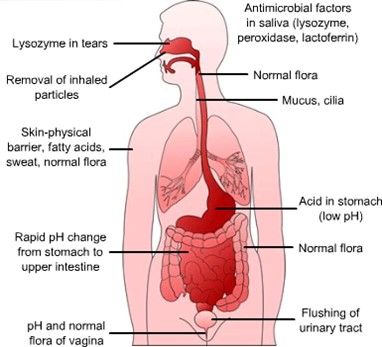
UHI / CC0
- Antimicrobial factors in saliva (lysozyme, peroxidase, lactoferrin)
- Lysozyme in tears
- Removal of inhaled particles from the nose
- Normal flora in the throat
- Mucus, cilia
- Skin is a physical barrier, fatty acids, sweat and normal flora
- Rapid pH change from the stomach to the upper intestine
- Normal flora in the gut
- Flushing or urinary tract
- pH and normal flora of the vagina
Quiz
Complete the table below and click on the submit button to check your answers.
| Organ | Secretion | Immune action |
|---|---|---|
| Sweat | Cell loss from surface of skin, acid pH, sweat flushes surface | |
| Tears | Tears contain lyzozomes to kill microbes | |
| Mucus | Cilia (hairs) prevent organisms entering lungs, mucus traps foreign bodies, cilia move foreign bodies upwards | |
| Stomach acid and bile acid | Stomach acid and other digestive secretions kill microbes |
Second line defences
First line defences provide non-specific physical or chemical barriers to potentially pathogenic microbes, but any break in this line of defence, such as damage to the skin or mucous membranes, permits the entry of organisms into the tissues.
Following physical damage affecting the surface or interior of the body such as cuts and abrasions, amputations or burns, micro-organisms have direct access to the tissue fluids and blood. It is essential that the body has a range of effective internal defences against invading micro-organisms.
These second line defences include:
- blood clotting
- fever
- inflammation
- complement proteins and interferons
- phagocytosis
Non-specific defences
Blood clotting and fever
Platelets (thrombocytes) are not cells, but fragments of large cells called megakaryocytes. They stick together and form a plug at the site of injury, preventing further loss of body fluids, and mending the first line of defence against pathogens. At the same time, proteins in blood plasma known as coagulation (clotting) factors initiate a cascade to form fibrin strands which help to plug up any break in the damaged epithelium.
Fever is a defence mechanism found in vertebrates where the internal body temperature rises above the normal 37º C. This rise in temperature inhibits pathogenic growth.
UHI / CC0
(Click image to toggle animation on/off)
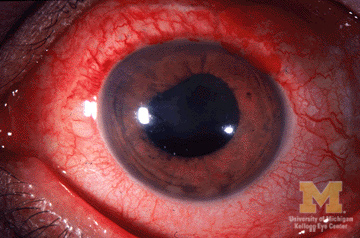
Inflammation
Inflammation is usually a local response to cellular damage by microbes or by physical or chemical agents, such as a scratch or substance that has irritated the skin. The purpose of inflammation is to contain microbes or other foreign material close to the injury site in preparation for tissue repair. It involves platelet secretions, vasodilating chemicals (histamine, prostaglandins, leukotrienes), complement proteins, interferons and mast cells.
Symptoms of inflammation are:
- Redness
- Heat
- Swelling
- Pain
The inflammatory response
Injury creates a sequence of events known as the inflammatory response:
- Damaged cells release chemicals such as histamine from mast cells.
- This causes local vasodilation and increased capillary wall permeability.
- The resulting heat makes the environment unfavourable for microbes.
- It promotes healing, raises leukocyte mobility, and increases the metabolic rate of nearby cells.
- Plasma leakage causes oedema
- Blood clotting factors such as fibrin initiate a clotting cascade around the injury site.
- Neutrophils and macrophages are attracted to the injury site resulting in phagocytosis and pus formation.
Once microbes have been destroyed, the inflammation usually settles down. The pain associated with inflammation results from damage, pressure from the swelling, and stimulation of nerve fibres by toxic chemicals from the microbes.
UHI / CC0
(Click image to toggle animation on/off)
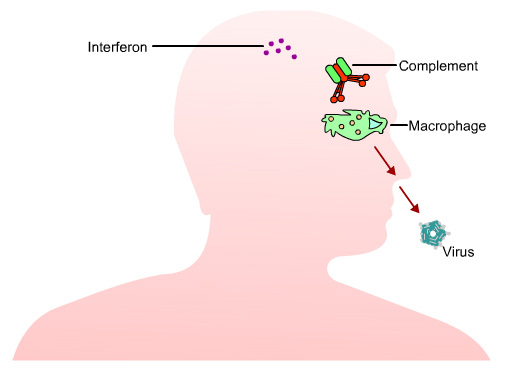
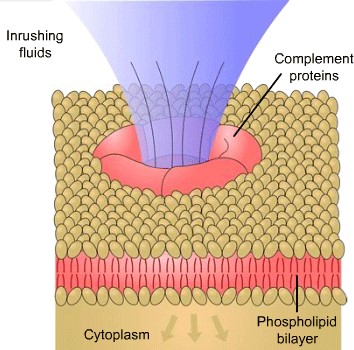
Complement proteins
Complement proteins work with (complement) antibody activity to eliminate pathogens. They are not antigen-specific and so are part of innate (built in) immunity, although some antibodies activate the complement system and so these form part of humoral immunity (antibody-mediated). They are produced by macrophages and liver cells and are present in the circulation as inactive molecules. Once activated, some complement proteins activate others, creating a cascade reaction.
Complement proteins stimulate inflammation and facilitate phagocytosis and pathogen destruction by tagging the outer surface of microbes for attack by phagocytes and leukocytes. They also attack some cells directly by binding to bacteria and opening pores in the membrane through which fluids and salt move. This swells and bursts the microbe cell.
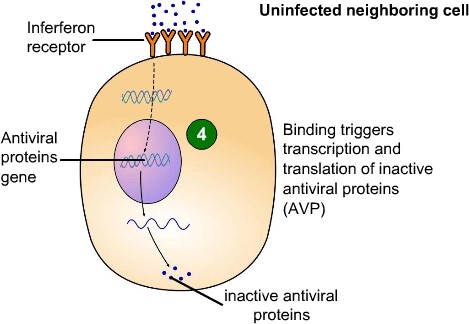
Interferons (cytokines)
Along with interleukins and growth factors, interferons are part of the family of cytokines, chemical messengers secreted by cells in the immune system. Interferons are cell-signalling proteins produced by cells infected with a virus. They are part of the non-specific immune system and are induced at an early stage in viral infection before the specific immune system has had time to respond.
The interferon binds to receptors on target cells and induces an antiviral state in these cells, although the cell that was originally infected will usually die. Interferons assist the immune response by inhibiting viral replication within host cells, activating natural killer cells and macrophages, and enhancing antigen presentation to lymphocytes.
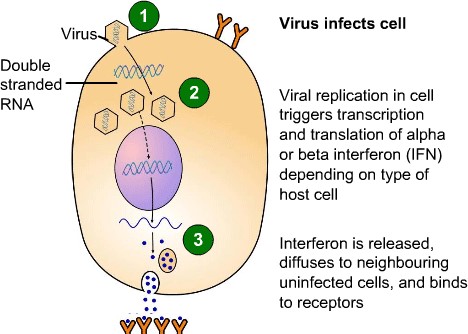
Viral replication in cell triggers transcription and translation of alpha or beta interferon (IFN) depending on type of host cell.
Interferon is released, diffuses to neighbouring uninfected cells and binds to receptors.
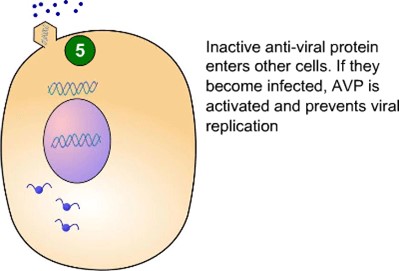
Inactive anti-viral protein enters other cells. If they become infected, AVP is activated and prevents viral replication.
UHI / CC0
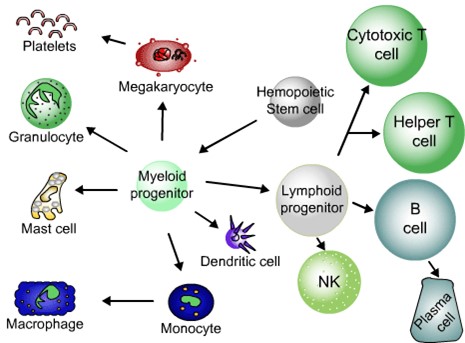
White blood cells (leukocytes)
The white blood cells (leukocytes) are important contributors to non-specific immunity and specific immunity. There are several types of leukocyte: lymphocytes and monocytes (known as agranulocytes), neutrophils, basophils and eosinophils (granulocytes). They are all produced in the bone marrow; some are present during inflammation as a second line of defence, and others provide cell-mediated (specific) immunity attacking specific pathogens.
These cells cause acute inflammation, and their cytoplasm is filled with granules, whereas other leukocytes are known as agranulocytes (no granules).
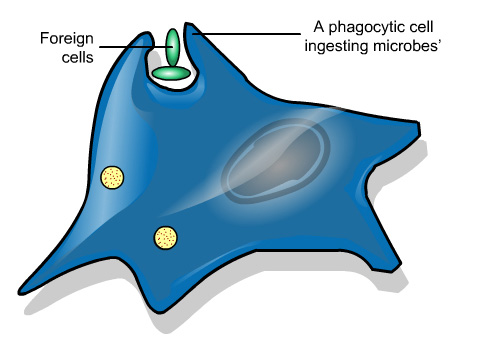
Neutrophils defend against bacterial or fungal infection through a process called phagocytosis. Phagocytes destroy microbial cells by engulfing and digesting them, and also remove dead cells and their remnants from damaged tissues. The localised accumulation of living and dead cellular material which results is called pus.
Neutrophils are present in large amounts in the pus of wounds but are unable to renew the intracellular lysosomes used in digesting microbes and die after phagocytosing a few pathogens.
Eosinophils primarily deal with parasitic infections and are also the predominant inflammatory cells in allergic reactions. They also counteract the effect of histamine.
Basophils release histamine causing inflammation in response to microbes and allergens. Basophils found in the tissues are called mast cells, which also release histamine.
Monocytes are also phagocytes but live longer than neutrophils. They also present pieces of pathogens to T cells so that an antibody response may be mounted. This means that pathogens can be recognized again and killed. Monocytes also cause inflammation as part of the immune response.
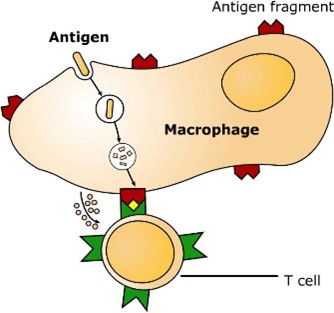
Monocytes eventually leave the bloodstream, enter the body tissues and mature into phagocytic macrophages. These remove dead cell debris as well as continuously searching for pathogens, engulfing and destroying them. Small fragments of the antigen are then displayed on the outer surface of the macrophage membrane. These antigens are recognised by T cells, which latch onto them and destroy them.
Leukocytes: Natural killer cells and B and T lymphocytes
Lymphocytes are more common in the lymphatic system than in the blood and are essential for cell-mediated and humoral (antibody) defence mechanisms. Natural killer cells (NK cells) are a type of lymphocyte and form part of the innate immune system that we are born with. They play a major role in viral infections and kill by releasing proteins which cause the target cell to die.
There are two other types of lymphocytes: B cells and T cells.
UHI / CC0
Hemopoietic stem cell > Myeloid progenitor >
- Granulocyte
- Mast cell
- Dendritic cell
- Megakaryocyte > Platelets
- Monocyte > Macrophage
- Lymphoid progenitor >
- Cytotoxic T cell
- Helper T cell
- B cell > Plasma cell
- NK
Once matured in bone marrow, B lymphocytes enter the blood and lymphatic circulation. B cells divide, forming plasma cells and B memory cells. Plasma cells make and release a large number of antibodies which are released into the blood. B memory cells live for months or years and retain the ability to produce an antibody from memory if the same pathogen is met again.
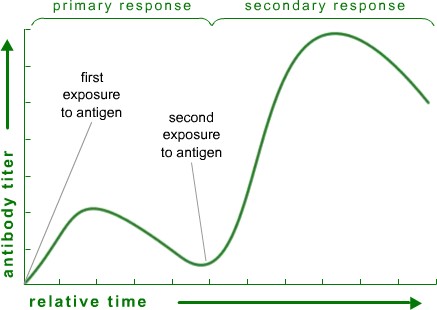
When first infected, the antibody level does not begin to increase until approximately 7-10 days after infection when it rises slowly to a low peak (primary response), then gradually declines but never returns to zero. The immune system, therefore, has a "memory". Once the immune system has produced a specific type of antibody or reactive B cell, it is capable of producing more of the antibody or activated B cell more rapidly and in larger amounts. On subsequent exposure to the same micro-organism, the level of antibody rises within 24 hours and remains high, referred to as a secondary or memory response.
UHI / CC0
Antigens are chemicals on the surface of a cell. The immune system checks cells and identifies them as “self” or “non-self”.
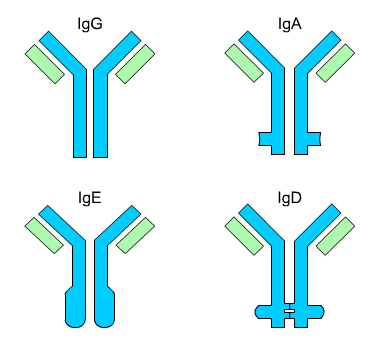
Antibodies bind to specific antigens in a lock-and-key fashion, forming an antigen-antibody complex. Antibodies are a type of protein molecule known as immunoglobulins, of which there are five types: IgG, IgA, IgD, IgE and IgM.
These recognize and bind to antigens and then inactivate them. Antibodies are specific to each antigen – they will only „fit‟ and lock onto the antigen that they were produced to fight.
UHI / CC0
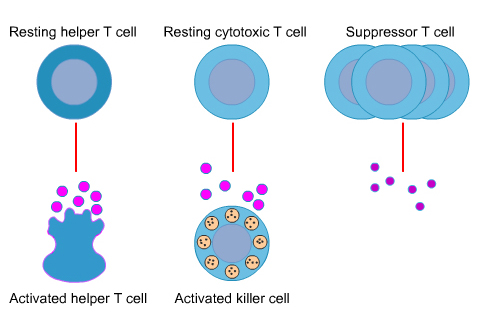
T cells migrate from bone marrow to the thymus gland and differentiate into helper T cells and cytotoxic T cells, offering cell-mediated immunity in the blood and lymph. Helper T cells activate and support other immune cells: they help in the development of plasma cells from B cells and assist in antibody production. Even after phagocytosis microbes may not be killed, but survive and multiply in macrophages. Helper T cells recognize macrophages containing intracellular bacteria through antigen receptors on the cell surface and help macrophages to kill bacteria by synthesising cytokines, chemicals which stimulate bacterial killing mechanisms of macrophages.
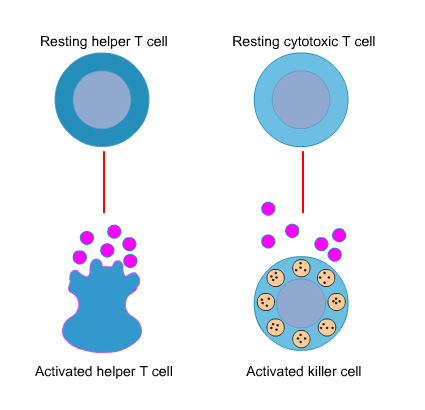
UHI / CC0
The principal role of cytotoxic T cells (also called Killer T cells) is to seek out and destroy body cells which display foreign antigens on their surfaces. When a virus infects a cell, it leaves a viral antigen on the cell surface. Cytotoxic T cells sensitised to this antigen bind to the infected cell and destroy it, limiting the multiplication and spread of a virus. Natural killer cells, another type of lymphocyte, also kill microbes in this way.
UHI / CC0
(Click image to toggle animation on/off)
Suppressor or regulatory T cells are responsible for reducing the level of immune response when the antigens have been destroyed. They are also believed to have a role in preventing the immune system from generating an immune response against normal body cells. They act as a natural “braking” system for our immune response.
UHI / CC0
Quiz
Specific immunity
Non-specific immunity involves general responses to any type of pathogen, such as inflammation. Specific immunity consists of two components which are both activated when the body is exposed to an antigen. Activation generally occurs in the lymph nodes or other lymphatic tissues.
Humoral (antibody-mediated) immunity is regulated by B cells and the antibodies they produce to inactivate or destroy antigens. It is known as humoral immunity as the B cells originate from the bone marrow of long bones such as the humerus. There may be up to one million different types of B cell in the body.
Cell-mediated immunity is controlled by T cells and involves the destruction of pathogens. Specific T cells are sensitised by certain antigens; no antibodies are secreted but a sub-group of T cells recognise and bind to the antigen on the surface of cells infected with microbes, and kill the cell.
Overview of cell-mediated immune function
Because our immune system recognizes that the body has been infected previously with a particular organism, this implies...
(“I’ve seen this antigen before”)
(“It doesn’t belong to me”)
(“I know exactly what this foreigner is”)
(“I know how to kill this foreigner”)
An immune response must recognise a micro-organism as foreign and distinct from our own cells, respond to a micro-organism by production of specific antibodies and lymphocytes, and mediate the elimination of micro-organisms.
An agent which creates an immune response is called an immunogen. The term antigen is applied to a substance which reacts with an antibody.
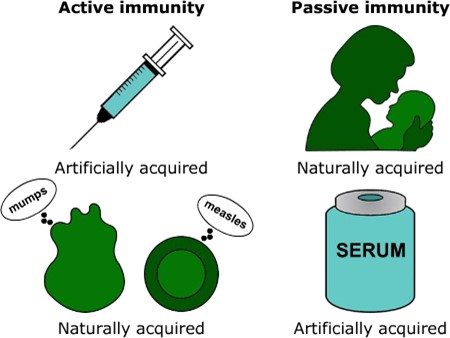
Types of Immunity
Immunity can be inherited, created within the body, or received in a vaccine
Naturally acquired
Active immunity
Active natural immunity occurs in response to infection. It is called adaptive immunity as the immune system must adapt itself to previously unseen molecules. Following recovery from certain infections with a particular micro-organism, individuals are less likely to develop an infection with the same organism as antibodies against that micro-organism have been produced and retain a memory (B memory cells) for an extended period of time, possibly for life. This form of protection is called immunity and an individual is said to be immune to that organism. Having immunity through infection is called active natural immunity.
Passive immunity
A non-immune individual may be immune genetically through the transfer of antibodies or lymphocytes from an immune individual, such as that between a mother and foetus, or through IgA antibodies in breast milk. This is called passive natural immunity, although it is usually temporary.
UHI / CC0
Artificially acquired
Following treatment with a vaccine, we can also acquire immunity.
Active artificial immunity...is when antigens (microbes) in small amounts are injected which stimulates the body’s own immune system to react, creating long term immunity.
Passive artificial immunity...is when “ready formed” immunoglobulins (antibodies) are injected directly into a patient – this provides immediate, but short-term immunity.
Quiz
Now it's time to test your knowledge of the lymphatic system.
You might want to take some time to read your notes, draw diagrams or watch the animations again before you test yourself!
Summary
You have completed your study of the Lymphatic System.
You should now have a good knowledge and understanding of the anatomy and physiology of the Lymphatic System.
You should be able to...
- Describe the organization of the lymphatic system and list its organs.
- Explain what lymph is and how it travels around the body.
- Describe the functions of the immune system Explain the differences between different types of immunity.
- Explain how the immune system works.
 UHI / CC0
UHI / CC0



 I
I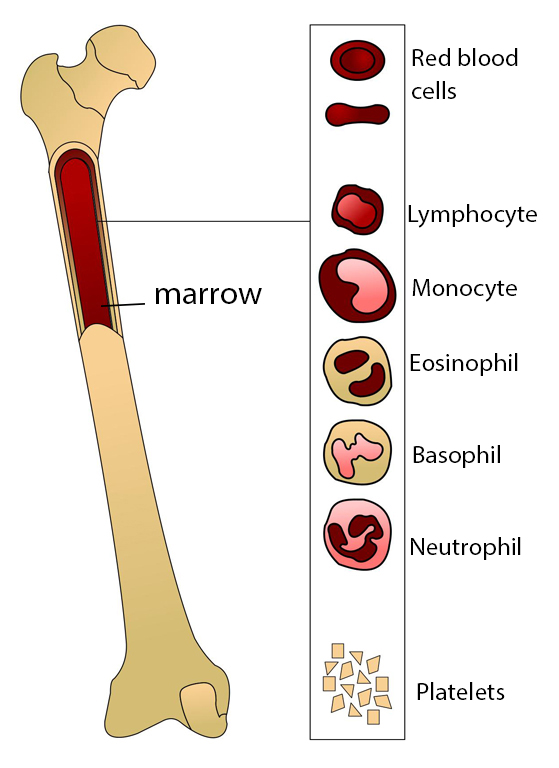
 response.jpg?1607009847979)