Introduction
You might work through this system over several weeks, days or hours, but to enhance your learning and enjoyment make sure you break it up into bite-size chunks.
Here are the sections of the reproductive system:
Make notes as you study each section, and interact fully with the activities – watch the animations and complete the quizzes.
Take a break at the end of each section– resting your eyes from the computer screen, getting some fresh air or taking a coffee break will improve your ability to focus on your study and take in information.
Give yourself time to think about what you have learned, and time to absorb and understand it.
 UHI /CC0
UHI /CC0
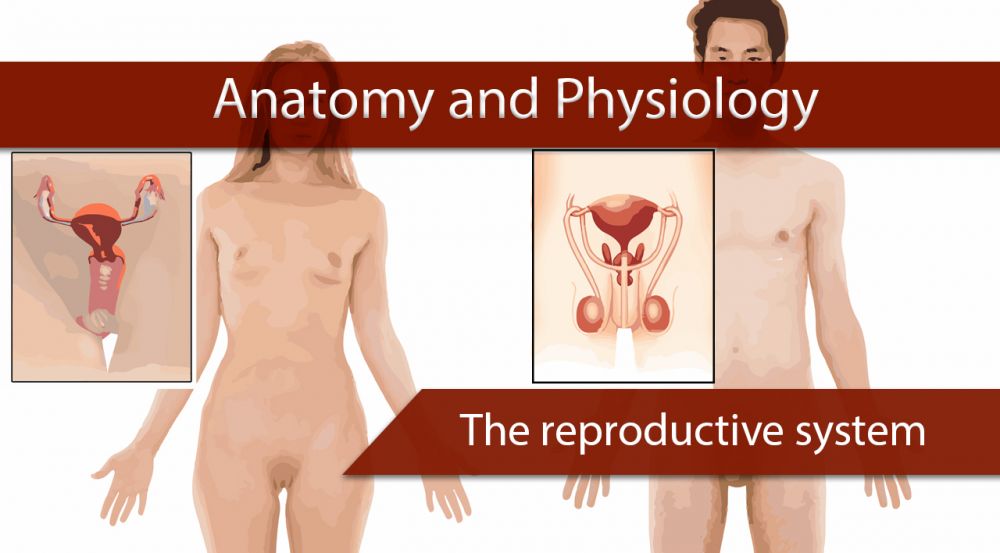
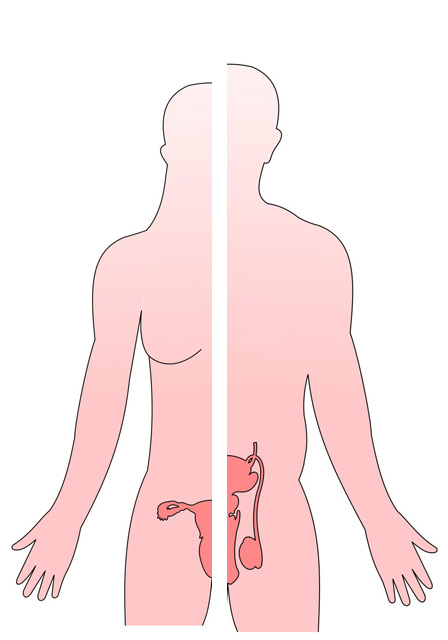
The reproductive systems
The structure and the function of the organs of the male and female reproductive systems differ, but both male and female reproductive organs are known as gonads. These produce reproductive cells called gametes. The male produces spermatozoa in the testes and the female produces ova in the ovaries. Each gamete contains chromosomes which carry genes from which offspring inherit their parents’ characteristics.
UHI / CC0
- Urinary bladder
- Ureter
- Seminal vesticle
- Prostate gland
- Accessory gland
- Vas deferens
- Erectile tissue
- Epididymus
- Erectile tissue
- Testes
- Glans penis
UHI / CC0
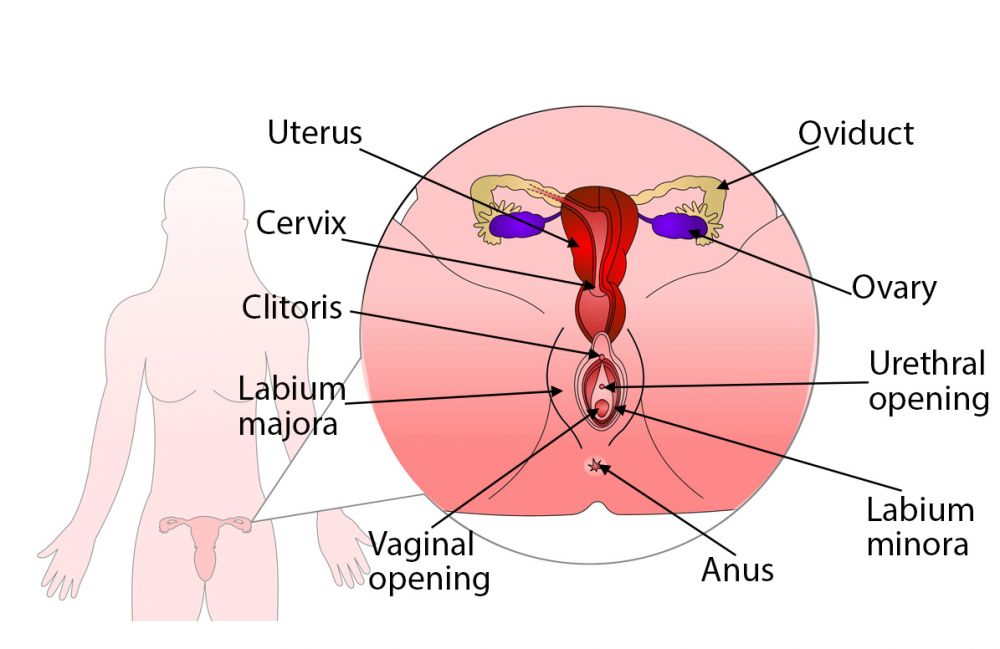
- Uterus
- Oviduct
- Ovary
- Cervix
- Clitoris
- Urethral opening
- Labium majora
- Labium minora
- Vaginal opening
- Anus
Spermatozoa and ova are formed by the process of meiosis. Following fertilisation, a zygote formed from the joining of the sperm and ova (egg) is produced, containing the full complement of 46 chromosomes from both parents. It embeds itself in the endometrium of the uterus and develops from a foetus into a baby over approximately 40 weeks. This ability to reproduce is enabled by the structure and physiology of each reproductive system.
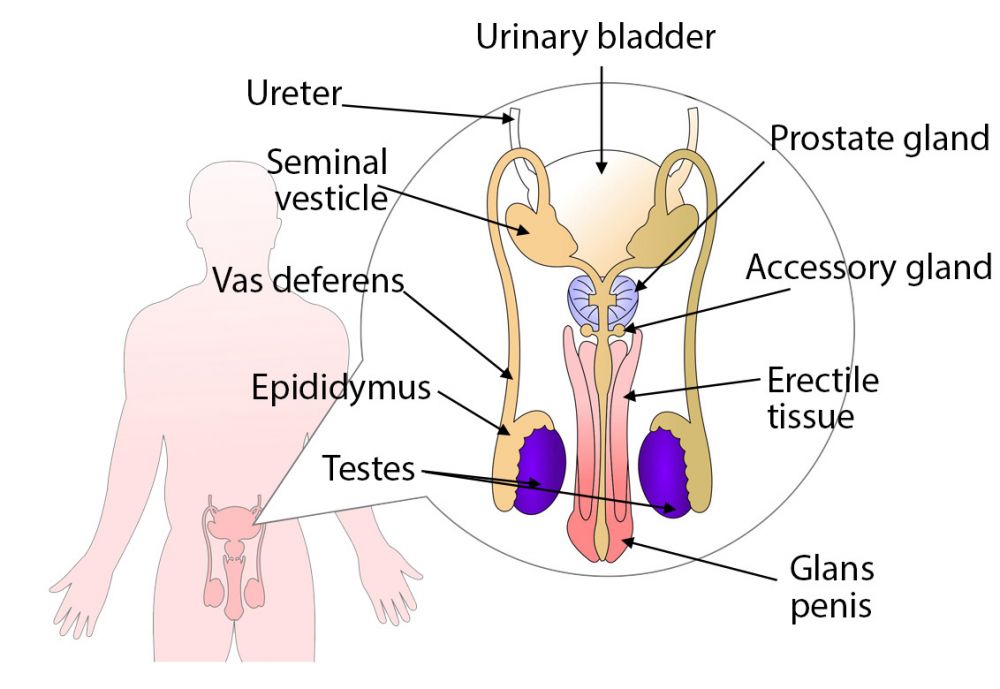
Anatomy of the male reproductive system
External structures of the male reproductive system include the penis, scrotum and testicles.
The penis is the organ used for sexual intercourse. The tube that transports semen runs through the penis and the opening is found at the tip of the glans penis. The scrotum is a pouch-like sac that lies behind the penis. The testicles, or testes, are found inside the scrotum. The scrotum allows the testes to remain slightly cooler than the rest of the body, which is essential for sperm development.
The testicles, normally two, are found in the scrotum. They are secured by the spermatic cord and produce the primary male sex hormone testosterone, which is required for generating sperm.
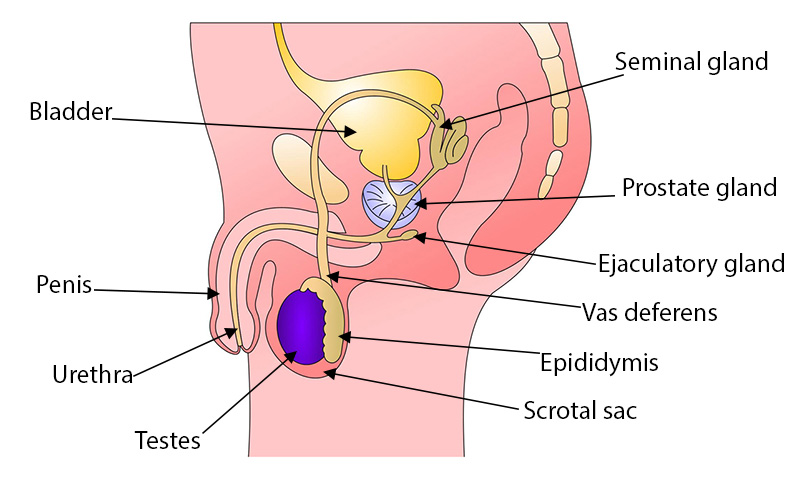
UHI / CC0
- Urinary bladder
- Seminal gland
- Prostate gland
- Ejaculatory gland
- Vas deferens
- Epididymus
- Scrotal sac
- Testes
- Urethra
- Penis
The internal structures include the vans deferens, ejaculatory ducts, urethra, prostate gland and seminal vesicles. Within the testes, coiled tubes called seminiferous tubules produce sperm cells (spermatogenesis). The tubules combine to form one larger tubule which is repeatedly folded over and tightly packed into a mass called the epididymis. This leaves the scrotum as the vas deferens.
The vas deferens transports mature sperm from the testes to the ejaculatory duct and urethra for ejaculation. The seminal vesicles are pouches lying behind the bladder. The vas deferens and seminal vesicles fuse to form the ejaculatory ducts which empty semen into the urethra. The urethra also carries urine from the bladder.
The prostate gland lies in the pelvic cavity behind the symphysis pubis. It secretes a milky fluid which makes up approximately 30% of seminal fluid and a clotting enzyme which thickens the semen in the vagina so it may remain in the cervix.
Functions of the male reproductive system
The functions of the male reproductive system are:
- Formation of spermatozoa, required for the reproductive process
- To maintain and transport sperm
- To produce and secrete the male sex hormone testosterone.
UHI / CC0
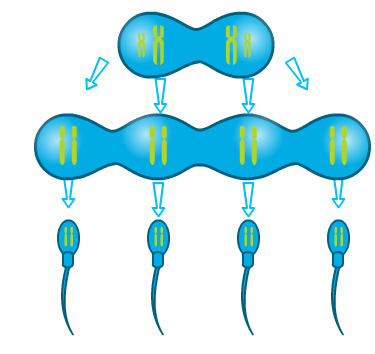
Spermatogenesis
The purpose of spermatogenesis is to produce the male gametes, spermatozoa, to fertilise the oocyte (ovum) of the female and produce a zygote, which develops into a foetus.
There are 23 chromosomes in each of the male and female gametes, and when joined together through fertilisation, the zygote has 46 chromosomes carrying all the genetic information inherited from the parents.
Spermatozoa are produced in the seminiferous tubules of the testes and stored in the epididymis where the spermatozoa mature. For spermatogenesis to take place the temperature must be 2-3º centigrade lower than the body temperature, which is why the testes hang outside the body within the scrotum.
Spermatogenesis takes approximately 64 - 74 days, continuing from puberty for the lifespan of the male.
UHI / CC0
(Click image to toggle animation on/off)
Stages of spermatogenesis
There are two stages of spermatogenesis.
Stage 1: Mitosis
This is a process of cell division which takes place with Diploid cells (Spermatogonia) which are immature stem cells lining the seminiferous tubules of the testes. This results in some of the cells remaining as stem cells and others developing into Primary Spermatocytes.
Stage 2: MeiosisThis is a second type of cell division which only takes place during development of male and female reproductive cells (spermatozoa and ova). Meiosis I is the process in which Haploid cells (secondary spermatocytes) form as a result from primary spermatocytes dividing. Meiosis II is when spermatids are produced by the secondary spermatocytes.
The spermatids develop a head and a tail and mature into a spermatozoon (sperm cell).
UHI / CC0
Maturation and transportation of sperm
Sperm maturation occurs in the epididymis of the testes over a period of approximately twenty days. The sperm are bathed in epididymal fluid rich in proteins and ions, which contributes to sperm maturation. Sperm are stored here prior to ejaculation.
Spermatozoa travel down a muscular tube called the vas deferens, which contracts during ejaculation and moves sperm into the ejaculatory duct. Here, sperm are mixed with secretions from the seminal vesicles before entering the urethra for ejaculation through the glans penis.
UHI / CC0
(Click image to toggle animation on/off)
Hormones of the male reproductive system
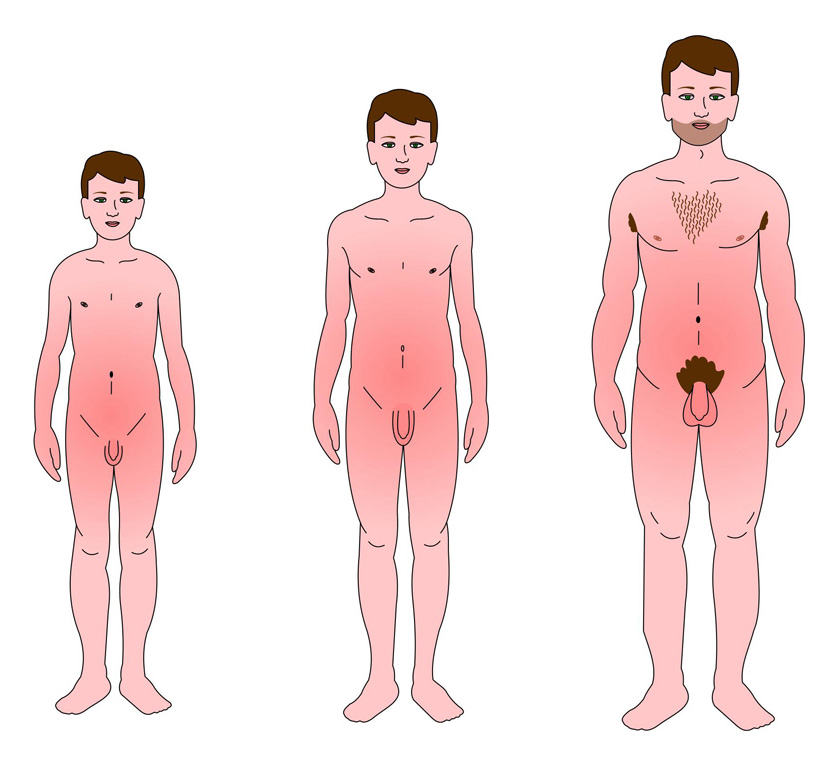
The testes secrete steroid hormones known as androgens which are responsible for male characteristics and behaviour such as facial hair, greater muscle mass, a deeper voice and slightly higher levels of aggression than in the female.
Along with growth hormone, testosterone promotes growth, particularly during puberty. At this time a number of changes in the male body occur including:
- Increase in male hormone levels
- Rapid increase in height and weight
- Hair growth is seen on the face, axilla (underarm), chest and pubic area
- Deepening of the voice
- The skin becomes thicker and more oily.
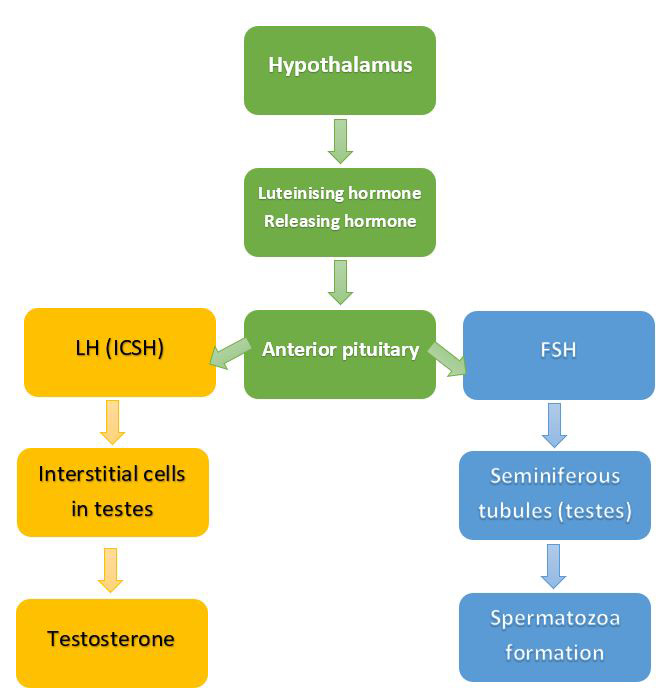
The hormones that stimulate the male reproductive organs are produced in the anterior pituitary gland. Their release is controlled by Gonadotropin Releasing Hormone (GnRH) which is produced in the hypothalamus.
The two hormones that are produced are Luteinising Hormone (LH) and Follicle Stimulating Hormone (FSH). In the male, luteinising hormone is also called Interstitial Cell Stimulating Hormone (ICSH). This hormone stimulates the interstitial cells in the testes to produce testosterone. FSH facilitates spermatozoa production by stimulating growth of the seminiferous tubules of the testes.
 UHI / CC0
UHI / CC0
The hormone Inhibin stops the release of FSH which leads to a reduction in the production of spermatozoa. This process occurs by negative feedback to the anterior pituitary gland once the required level of spermatogenesis has been achieved.
 UHI / CC0
UHI / CC0
Hormones of the male reproductive system flowchart
Quiz
Name the areas of the diagram.
Female reproductive system
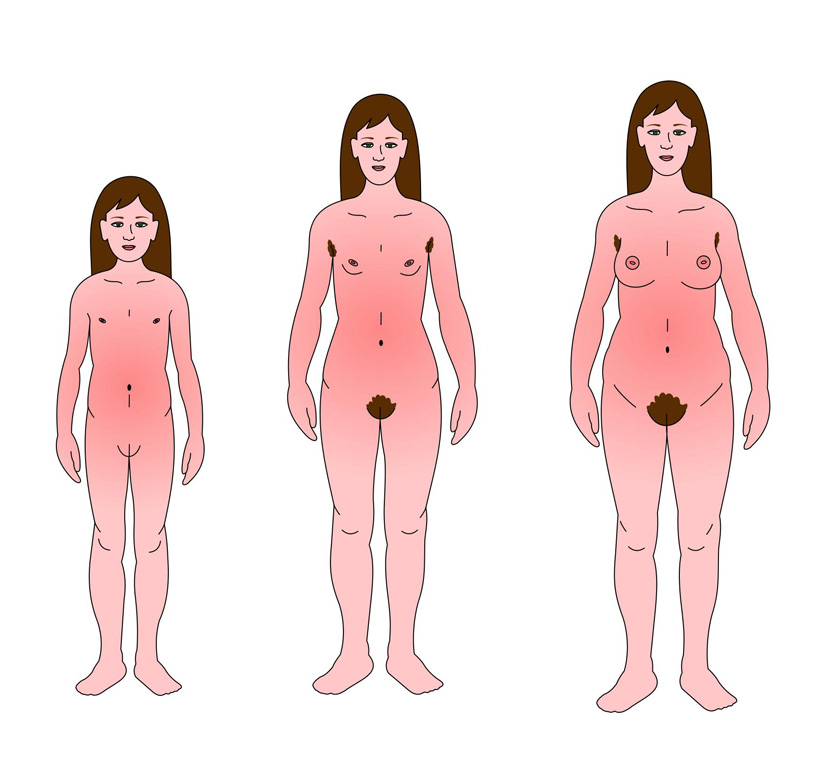
The change from childhood to womanhood when females become fertile is known as puberty. Puberty in the female generally takes place at the start of the teenage years or slightly earlier.
The following changes occur during puberty in the female:
- A spurt in the growth rate
- Sexual organs become fully developed
- The body gains fat deposits
- Breasts develop
- The pelvis widens
- Pubic and axilla (underarm) hair starts to grow
- Menstruation begins.
 UHI / CC0
UHI / CC0
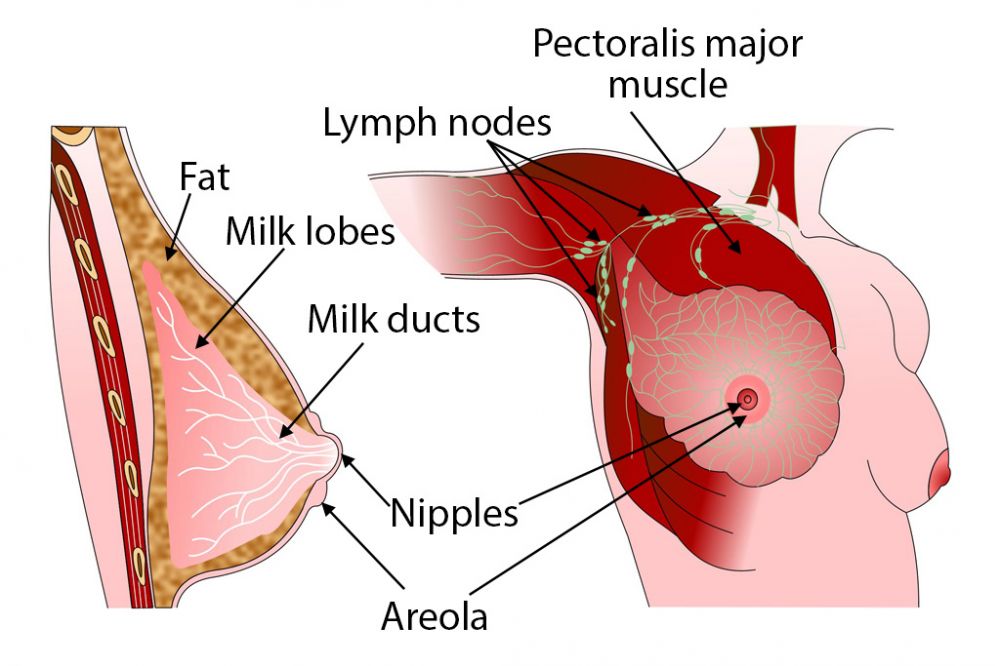
Breasts
The breasts are also known as mammary glands and although present in the male, they do not develop. The function of the breasts is to produce milk following childbirth, known as lactation.
The breast is comprised of lobes of glandular tissue, and each lobe has milk ducts leading to the nipple which widen and form reservoirs for milk. Another component of the breast is the connective tissue that supports the lobes and ducts.
Breast development in the female takes place during puberty. The growth spurt is under the influence of the female hormones oestrogen and progesterone, which are secreted by the ovaries and lead to a build up of fat within the breast resulting in the breasts’ fullness.
The breasts grow in size during pregnancy due to further stimulation by the female hormones.
The anterior pituitary gland produces the hormone prolactin after childbirth which stimulates milk production.
The posterior pituitary gland produces oxytocin which releases the milk in response to the sucking action on the nipple by the baby.
Anatomy of the female reproductive system
External structures of the female reproductive system include the vulva, clitoris, hymen and vestibular glands.
The vulva is comprised of the labia majora and minora. The labia majora is two large outer folds of skin which join in front of the symphysis pubis and merge with the perineum at the back, and contain a number of sebaceous glands.
The labia minora has two smaller folds of skin which lie between the folds of the labia majora and also contain numerous sebaceous glands. The cleft between the labia minora is known as the vestibule. Ducts of the greater vestibular glands, the vagina and urethra open into the vestibule.
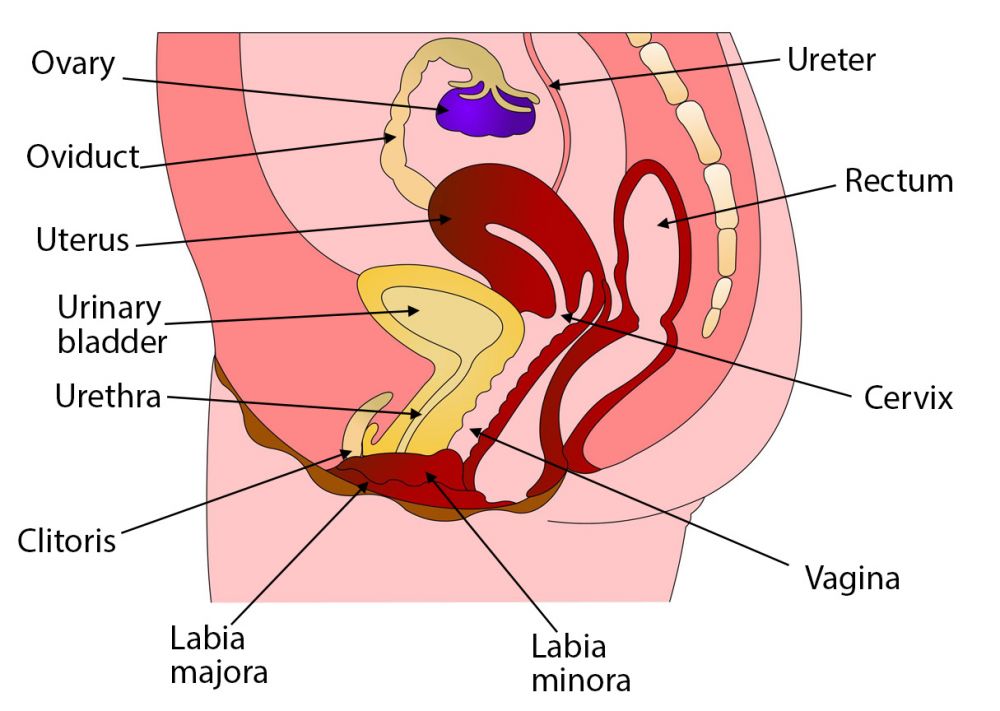
UHI / CC0
- Ureter
- Oviduct
- Ovary
- Rectum
- Uterus
- Urinary bladder
- Cervix
- Urethra
- Clitorus
- Labia majora
- Labia minora
- Vagina
The vestibular glands contain ducts and keep the vulva moist by secreting mucous. They are also known as the Bartholin’s glands, with one located at either side of the opening to the vagina.
The vagina is a hollow tube connecting the external genitalia with the internal genitalia. It is located between the bladder at the front and the rectum at the back.
The clitoris is the female equivalent of the male penis, containing sensory nerves and erectile tissue.
The hymen is a thin layer of mucous membrane that partially covers the entrance to the vagina but allows passage of menstrual flow.
Uterus and fallopian tubes
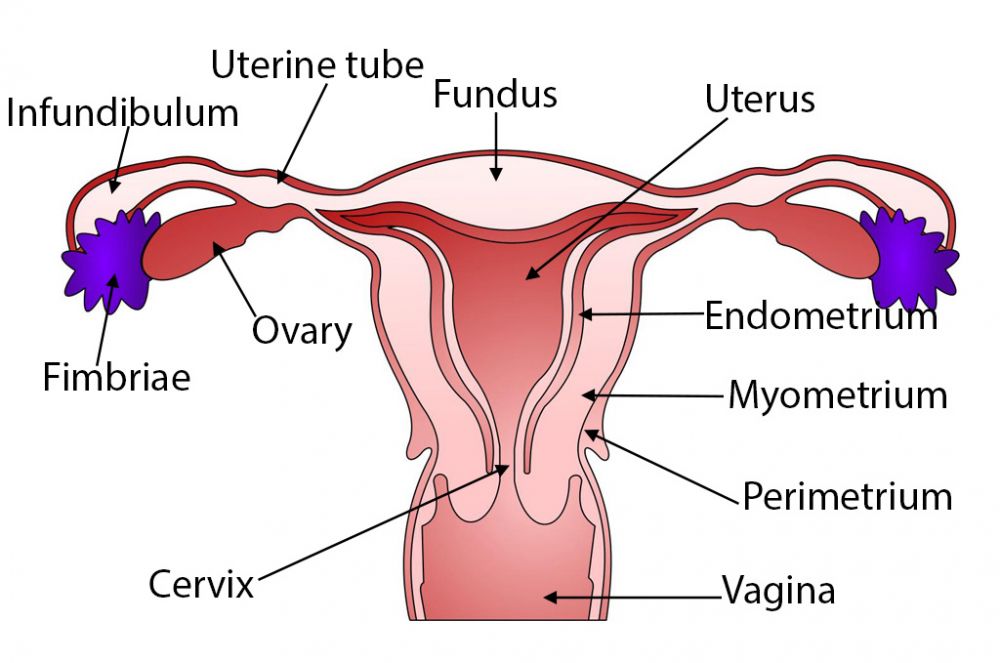
UHI / CC0
- Infundibulum
- Uterine tube
- Fundus
- Uterus
- Fimbriae
- Ovary
- Endometrium
- Myometrium
- Perimetrium
- Cervix
- Vagina
Fallopian tubes
The fallopian tubes extend one from each side of the upper part of the uterus. Each tube is approximately 10cm long and made up of three layers – an outer membrane, a middle layer of muscle and an inner layer of ciliated epithelium.
At the end of each fallopian tube are finger-like tentacles called fimbriae which lie directly above each ovary. The fimbriae channel the ovum towards the fallopian tube once it has been released by one of the two ovaries. The ovum is then wafted along the fallopian tube to the uterus by the movement of the cilia. Fertilisation usually takes place within the fallopian tube.
The uterus
The uterus is a hollow, muscular pear-shaped organ. There are three parts to it:
- the fundus is the dome-shaped part above the openings of the uterine tubes
- the body is the main part of the uterus
- the cervix is the ‘neck’ of the uterus protruding into the vagina.
The uterus wall has three layers:
- The perimetrium (outer layer)
- The myometrium (middle, smooth muscle layer)
- The endometrium (inner layer). This has two functional layers.
UHI / CC0
The ovaries
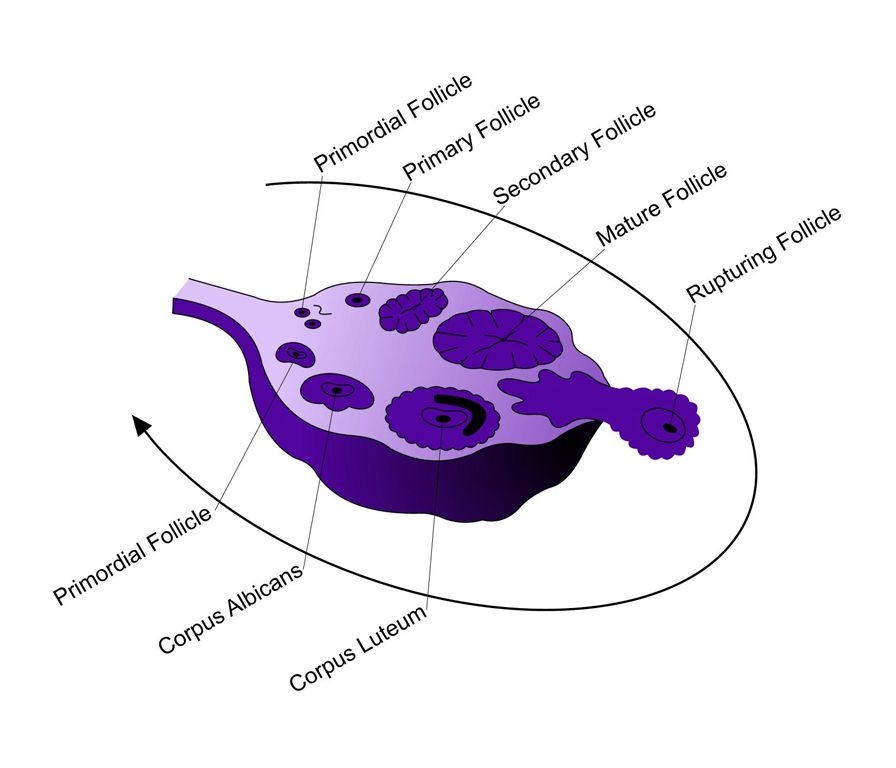
The ovaries are the female gonads and are situated directly below the fallopian tubes. There are two ovaries, approximately 3cm long by 2cm wide, which lie either side of the uterus. Their surfaces are smooth but gradually wrinkle as ova are released. At birth, each ovary of a female contains around 200,000 immature follicles.
Each follicle contains an immature egg called a primary oocyte. After puberty, oocytes develop into ova (eggs) at the rate of one every month until the menopause. During this time, approximately 400 will mature and divide before release during ovulation.
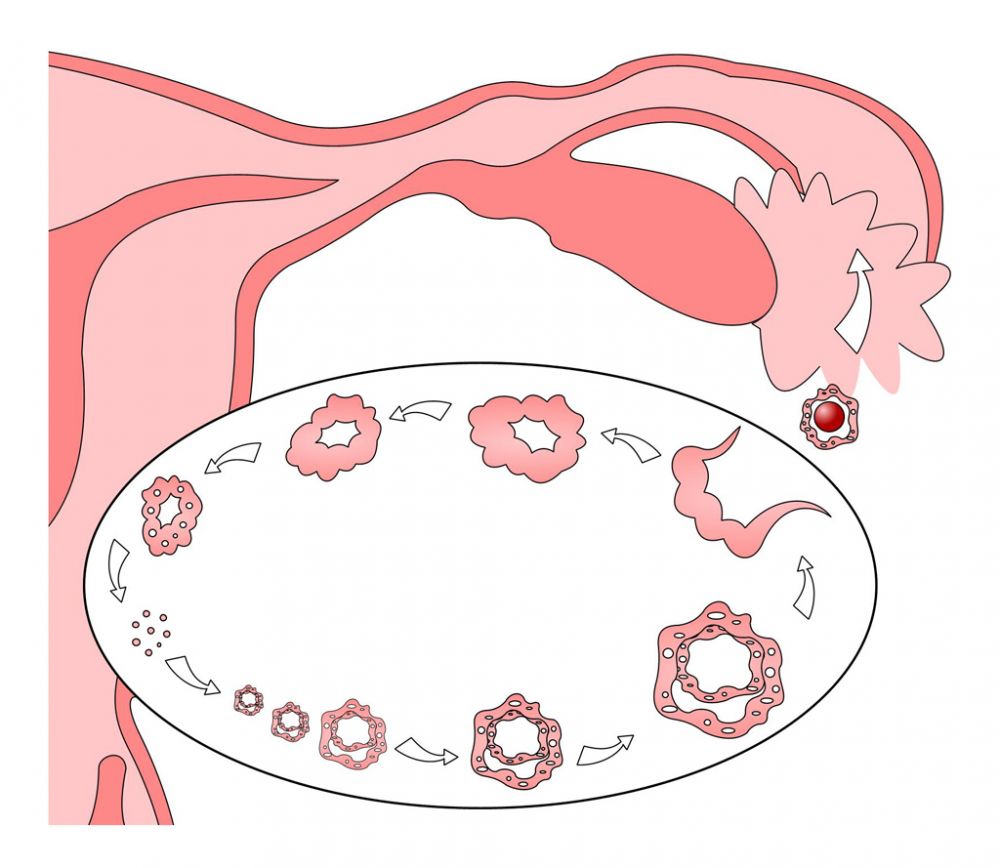
The cycle of a developing ovarian follicle
UHI / CC0
Primordial follicle > Primary follicle > Secondary follicle > Mature follicle > Rupturing follicle
Corpus luteum > Corpus albicans > Primordial follicle...
Quiz
Name the areas of the diagram.
Functions of the female reproductive system
The female body acts as a receptacle for the male sperm, providing the ideal environment for fertilisation between the ova and sperm, and for the growth of the foetus. The pelvic area of the female body is designed to facilitate childbirth, and the breasts produce milk for the newborn baby.
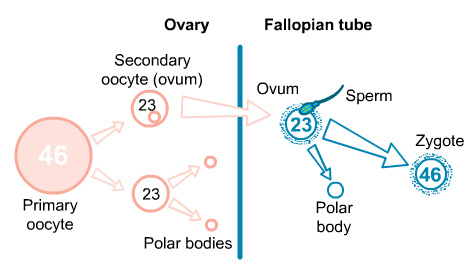
Formation of ova
The process by which the maturing oocyte divides is known as meiosis. The primary oocyte with its full complement of 46 chromosomes divides to form a secondary oocyte called the ovum and a smaller polar body. The polar body may divide again to form two polar bodies which disintegrate.
The secondary oocyte (ovum) contains 23 chromosomes, which divide just prior to ovulation to form another polar body, which only splits away if a sperm penetrates the ovum. If sperm penetrates the ovum, it adds its 23 chromosomes to those of the ovum bringing the number of chromosomes back to the normal number of 46.
UHI / CC0
(Click image to toggle animation on/off)
UHI / CC0
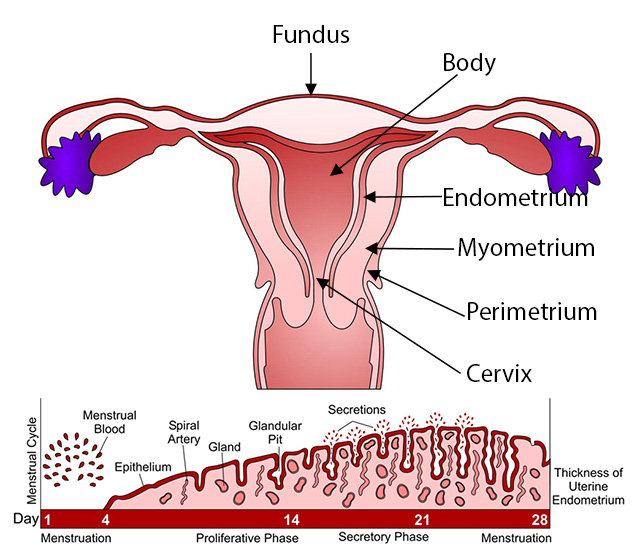
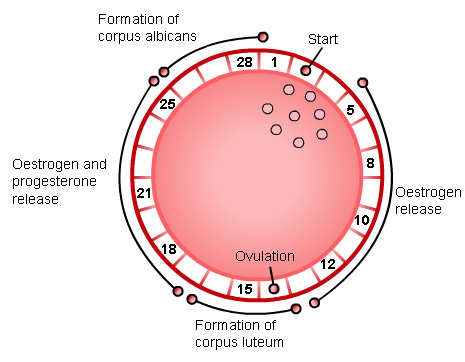
The menstrual cycle
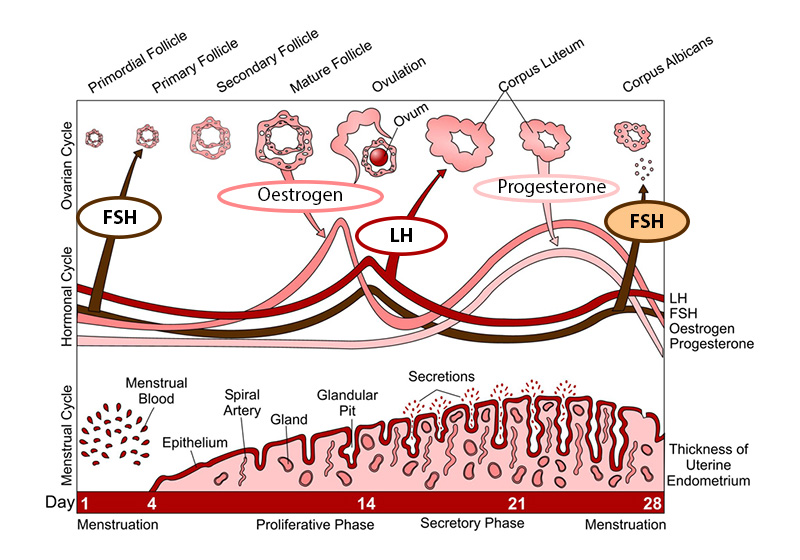
Menstruation occurs in women in regular cycles of approximately 26-30 days during the fertile years between puberty and the menopause. The cycle consists of a series of changes in the endometrium and ovaries, stimulated by changing levels of female hormones.
Every month a fertile woman ovulates, releasing an ovum. The menstrual cycle is the process through which the endometrium prepares to receive the ovum if it is fertilised. If it is not fertilised, both the unfertilised ovum and the endometrial lining of the uterus break down and shed at the start of the next menstrual cycle. The start of the first menstrual cycle is known as the menarche.
UHI / CC0
FSH: Release of Follicle Stimulating Hormone from the anterior pituitary prompts a follicle in the ovary to begin to develop.
Oestrogen: The maturing follicle releases oestrogen, which stimulates release of Luteinising Hormone (LH) from the anterior pituitary.
LH: LH stimulates ovulation, and the ovum is released from the follicle. LH also causes the ruptured follicle to turn into corpus luteum.
Progesterone: The corpus luteum secretes oestrogen and progesterone.
FSH: Folicle Stimulating Hormone begins to rise again, which prompts another follicle to begin maturation, and the ovian cycle begins again.
There are a number of changes which occur during the monthly cycle of a female between puberty and menopause. These changes are all part of the female reproductive cycle.
The pituitary (hormonal) cycle depicts the changing levels of Luteinising Hormone and Follicle Stimulating Hormone over a typical 28 day cycle. The hormonal cycle also illustrates the sex hormone cycle, with changing levels of oestrogen (oestradiol) and progesterone over a typical 28 day cycle.
The ovarian cycle follows the changes taking place in the ovaries, including development of ovarian follicles and the corpus luteum, and the release of an ovum (egg).
The menstrual cycle is also known as the endometrial cycle and follows the changes taking place in the endometrium, including menstruation and the thickening of the endometrial lining in readiness to receive a fertilized ovum.
The ovarian cycle (ovulation)
Stimulated by follicle stimulating hormone (FSH), several follicles enlarge around a fluid-filled cavity. Normally only one will grow to maturity each month. The enlarging follicle secretes the hormone oestrogen. Upon ovulation, the Graafian (mature) follicle bursts, releasing the ovum into the fallopian tube.
The ruptured follicle now becomes a glandular structure called the corpus luteum which secretes progesterone and oestrogen. If the ovum is fertilised, the corpus luteum will continue to produce the hormones. If no fertilisation takes place, the corpus luteum will only last another 10 days before collapsing to become the corpus albicans, which degenerates over time.
The egg is either fertilized, or lost during menstruation.
If fertilized, the ovum embeds in the endometrium and secretes a hormone called Human Chorionic Gonadotropin which ensures the continuation of the corpus luteum until the placenta begins to secrete oestrogen and progesterone.
If not fertilized, the ovum is secreted with the endometrium during menstruation.
UHI / CC0
The menstrual cycle (endometrial)
Days 1-5: The first day of menstruation is the start of each cycle when the endometrial lining built up during the previous menstrual cycle is shed as the menstrual flow.
Days 5-14: The rapidly maturing ovarian follicle releases oestrogen which stimulates the endometrium to thicken in preparation for the ovum.
Day 14: Luteinising hormone causes the mature Graafian follicle to rupture, releasing the ovum.
Days 14-16: The empty follicle forms the corpus luteum. This secretes oestrogen and progesterone which prepare the endometrium to receive the ovum. Fertilisation must take place during this stage.
Days 17-20: The ovum travels down the fallopian tube to enter the uterus.
Days 21-30: If the ovum is not fertilised the corpus luteum degenerates to form the corpus albicans and stops oestrogen and progesterone production. This causes the endometrium to break down and is lost as menstrual flow during the next cycle.
UHI / CC0
Hormones in the female reproductive cycle
There are five hormones involved in the female reproductive cycle. The hypothalamus is involved in initiating the menstrual cycle, by releasing Gonadotropin Releasing Hormone (GnRH). This stimulates the release of Follicle Stimulating Hormone (FSH) and Luteinising Hormone (LH) from the pituitary gland.
FSH is primarily responsible for stimulating maturation of the follicles in the ovary and oestrogen secretion, leading to ovulation. LH triggers ovulation, and transforms the Graafian follicle into the corpus luteum.
Following the release of LH and FSH, the maturing follicle secretes oestrogen and progesterone, giving a rise in these hormones in the second half of the cycle. This initially has a negative feedback effect on FSH production, but high levels of oestrogen prior to ovulation increase pituitary secretion of FSH and LH (a positive feedback effect), and FSH and LH levels peak immediately before ovulation.
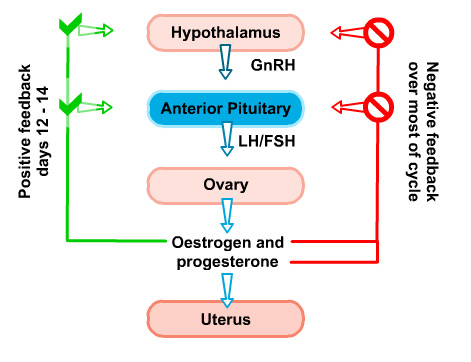
UHI / CC0
Human Chorionic Gonadotrophin (HCG)
A fertilised ovum secretes Human Chorionic Gonadotropin (HCG), which ensures the continued existence of the corpus luteum until such time as the placenta can take over the secretion of sufficient quantities of oestrogen and progesterone. In the absence of HCG, the corpus luteum atrophies (reduces in size), oestrogen and progesterone production declines, and the start of the next menstrual cycle is initiated with the shedding of the endometrial lining of the uterus.
Quiz
Fill in the blanks.
The menopause
The average age of the menopause is during the early fifties, but it may happen earlier or later in life. It marks the end of the period of fertility in women.
There are three stages to the menopause:
Pre-menopause – this is when the woman’s period becomes irregular and/or heavy.
Peri-menopause – the woman’s periods become more irregular and she may start to suffer symptoms such as hot flushes.
Post-menopause – this is the last and final stage, when the woman’s periods stop altogether.
As females reach the end of fertile years, the ovaries fail to produce oestrogen and progesterone. The loss of oestrogen can lead to atrophy of the urinary tract, hot flushes, night sweats, irritability, mood swings and loss of sex drive. Reduced levels of oestrogen may also contribute to osteoporosis as it is an anabolic hormone that increase bone tissue growth.
Test your knowledge
Now it's time to test your knowledge of the reproductive system. There are 10 questions to complete.
You might want to take some time to read your notes, draw diagrams before you test yourself!
Summary
You have completed your study of the reproductive system.
You should now have a good knowledge and understanding of the anatomy and physiology of the reproductive system. You should be able to:
- Identify and name the major anatomical parts of the male and female reproductive organs
- Discuss the functions of the male and female reproductive systems
- Discuss the hormones involved in the male and female reproductive systems and their effects in the body
- Describe the female ovarian cycle
If you think that your knowledge or understanding of any section of the reproductive system could be improved further, go back to the relevant sections and work through them again, taking time to make notes and complete the activities.
 UHI / CC0
UHI / CC0