Introduction
You might work through this system over several weeks, days or hours, but to enhance your learning and enjoyment make sure you break it up into bite-size chunks.
Here are the sections of the urinary system:
As you study the urinary system you will learn about:
- Structure of the urinary system
- The kidneys
- Kidney microstructure
- Formation of urine
- Regulation of water volume & blood pressure
- Micturition
Make notes as you study each section, and interact fully with the activities – watch the animations and complete the quizzes.
Take a break at the end of each section– resting your eyes from the computer screen, getting some fresh air or taking a coffee break will improve your ability to focus on your study and take in information.
Give yourself time to think about what you have learned, and time to absorb and understand it.
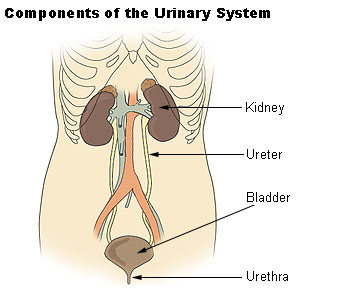
Structure of the urinary system
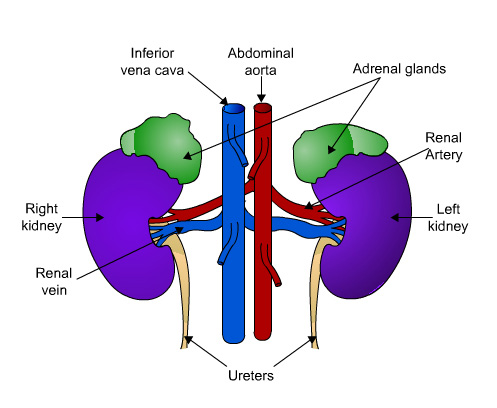
The urinary system is an excretory system consisting of two kidneys, two ureters, the bladder and urethra. The system maintains homeostasis of water and electrolyte balance (the amount of sodium and potassium ions) in the body, and removes many of the waste products of metabolism.
The balance between fluid intake and output is controlled by the kidneys, as water is the main constituent of urine.
The kidneys
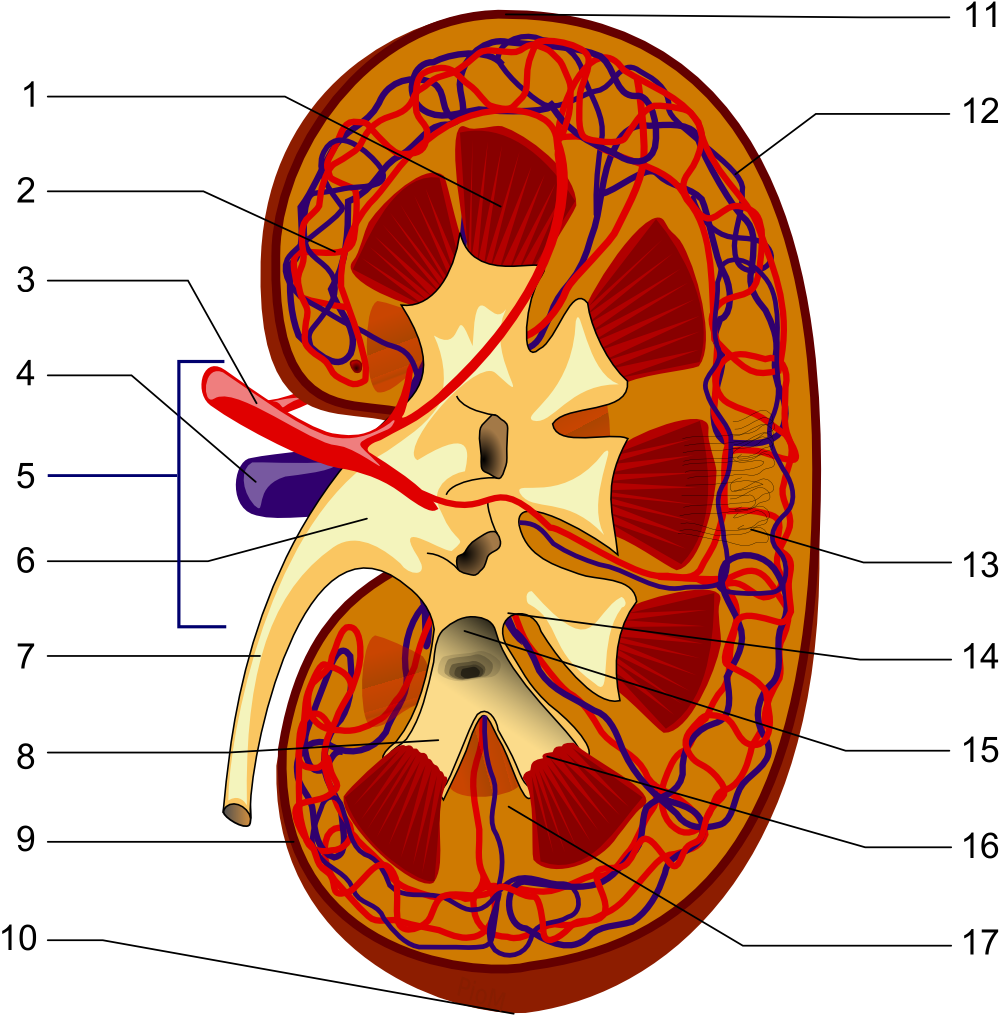
The kidneys are bean-shaped and are embedded in a mass of fat, lying on either side of the vertebral column just below the diaphragm. The adrenal glands sit on top of the kidneys. The aorta carries oxygenated blood from the heart to the renal arteries, and renal veins carry deoxygenated blood from the kidneys back to the inferior vena cava.
The hilum is the concave inner (medial) border of the kidneys where the blood and lymph vessels, the ureters and nerves enter or leave.
 UHI / CC0
UHI / CC0
Inferior vena cava
Abdominal aorta
Adrenal glands
Renal artery
Right kidney
Left kidney
Renal vein
Ureters
The function of the kidneys
The kidneys produce urine which contains many of the products of metabolic waste, including urea and uric acid and some drugs.
The kidneys have the following functions:
- formation and secretion of urine
- production of erythropoietin, a hormone that controls formation of red blood cells
- production and secretion of renin, an enzyme that helps to control blood pressure and blood volume.
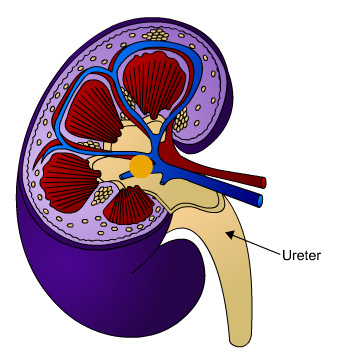
Key
- Renal pyramid
- Interlobular artery
- Renal artery
- Renal vein
- Renal hylum
- Renal pelvis
- Ureter
- Minor calyx
- Renal capsule
- Inferior extremity
- Superior extremity
- Interlobar vein
- Nephron
- Renal sinus
- Major calyx
- Renal papilla
- Renal column
(no distinction for red/blue (oxygenated or not) blood, arteriole is between capilaries and larger vessels)
The ureters
The ureters are tubes that carry urine from the kidney area called the pelvis to the bladder. Contraction of the muscular wall of the ureters moves urine by peristalsis.
The urine leaves the bladder by openings called sphincters. The internal sphincter is not under voluntary control, whereas the external sphincter which controls urine flow from the body, is under voluntary control, which is learned in childhood.
 UHI / CC0
UHI / CC0
Quiz
Now have a go at labelling the kidney. Match the terms below to the corresponding parts.
Microstructure of the kidneys
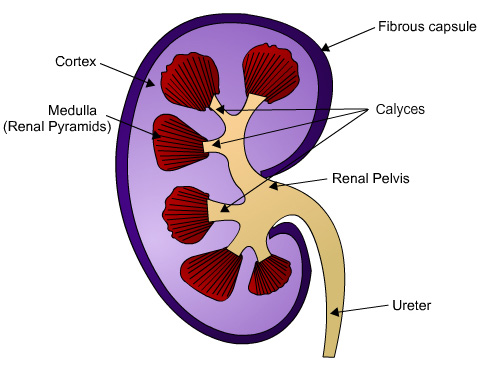
There are three areas within the kidney:
- a fibrous capsule surrounding the kidney
- the cortex, a reddish brown layer of tissue
- between the capsule and the inner medulla
- the medulla, containing conical- shaped renal pyramids.
The renal pelvis is a funnel-shaped structure that acts as a receptacle for the urine formed by the kidney. Urine passes through a papilla at the apex of each renal pyramid in the medulla into a calyx. Minor calyces join larger branches surrounding the apex of each renal pyramid and carry any urine formed through the pelvis into a ureter. Peristalsis in the smooth muscle of the pelvis propels urine through the ureters to the bladder.
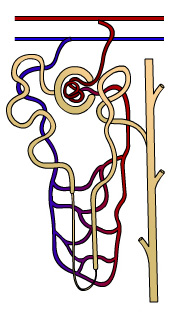
Nephrons – the functional unit of the kidney
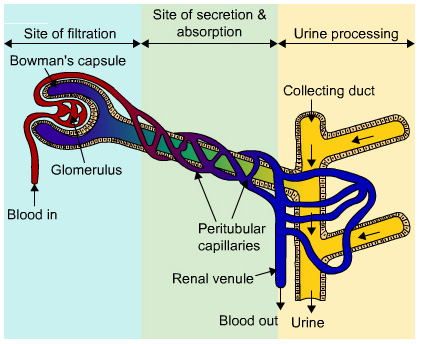
Each kidney is composed of over a million functional units called nephrons. Each nephron contains a glomerulus (a network of capillaries also known as the glomerular capsule) and a renal tubule which is approximately 3cm long and consists of a:
- Bowman’s capsule (cup-shaped structure contains the glomerulus)
- Proximal convoluted tubule (site of reabsorption and secretion)
- Loop of Henle (site of water reabsorption)
- Distal convoluted tubule (site of further reabsorption and secretion), and
- A collecting duct which unites with other ducts and empties into the calyces.
 UHI / CC0
UHI / CC0
Bowman's capsule, proximal convoluted tubule, loop of Henle, descending limb of loop of Henle, ascending limb of loop of Henle, distal convoluted tubule, and collecting duct.
Formation of urine
Urine forms in the kidneys and passes through the ureters to the bladder, where it is stored before it is excreted. A healthy adult will pass between one and two litres of urine a day. The three main processes of forming urine are:
- Filtration
- selective reabsorption
- secretion.
UHI / CC0
(Click image to toggle animation on/off)
Filtration
Filtration occurs between the semi- permeable walls of the glomerulus and the Bowman’s capsule. The glomerus is a network of blood capillaries through which water and small molecules can pass through (although most of these are reabsorbed later) but large molecules, such as blood cells and plasma proteins are too large and remain in the capillaries. The walls of the glomerular capillaries are more permeable than other capillaries. The substances that filter through into the Bowman’s capsule become known as the filtrate.
UHI / CC0
(Click image to toggle animation on/off)
Glomerular blood enters through the afferent arteriole, filtration occurs between the semi- permeable walls of the glomerulus and the Bowman’s capsule. Glomerular filtrate leaves while blood not being filtered passes through the efferent arteriole.
Regulation of filtration rate
Filtration is assisted by the difference in blood pressure between the glomerulus (the network of capillaries) and the glomerular capsule around it. A higher pressure is created in the glomerulus as a larger arteriole enters the capsule than the efferent arteriole leaving it. This creates a net filtration pressure which assists the filtration rate which needs to remain constant.
When blood pressure increases, a rush of blood flows into the glomerulus but a reflex constriction occurs in the muscle wall of the afferent (incoming) arteriole which prevents an increase in filtration rate. When blood pressure decreases the reverse occurs. This auto-regulatory mechanism is called myogenic as it depends on a muscular reflex in the afferent arteriole.
UHI / CC0
(Click image to toggle animation on/off)
The glomerular blood and glomerular filtrate are of a similar composition – the only difference is that large plasma proteins are unable to pass through the semi-permeable walls of the glomerular capillaries into the capsule.
The filtrate is made up of:
- water
- minerals and mineral salts (e.g. sodium, potassium, calcium, magnesium)
- glucose
- amino acids
- keto acids
- some hormones
- creatinine
- some toxins and drugs
- uric acid
- urea.
 UHI / CC0
UHI / CC0
Site of filtration:
Blood goes in, passes through the Glomerulus and Bowman's capsule.
Site of secretion & absorption:
Blood passes through pertubular capillaries to renal venule, blood out.
Urine processing:
Filtrate moves to collecting duct and exits as urine.
Quiz
Now have a go at identifying the parts of the nephron. Match the terms below to the corresponding parts.
Selective reabsorption
Selective reabsorption is the process by which the substances needed by the body to maintain water balance and blood pH are reabsorbed from the glomerular filtrate as it travels through the rest of the nephron in the kidney. Reabsorption occurs by a combination of diffusion, active transport and osmosis. Active transport uses energy to transport substances back into the blood against their concentration gradient, whereas osmosis is movement of water from a higher to a lower concentration gradient.
In the glomerular filtrate, glucose and amino acids are almost all reabsorbed by the time they reach the Loop of Henle. Amino acids and salts (sodium chloride) are also reabsorbed by active transport and nitrogenous waste (urea) is secreted.
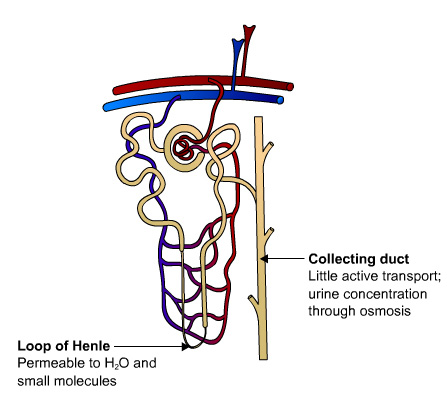
At the Loop of Henle (also known as the medullary loop), further reabsorption of water and salts takes place but its main role is to create a high osmotic pressure in the loop so that more water is reabsorbed. 80% of the original water in renal fluid has been reabsorbed by the time it reaches the distal convoluted tubule. Potassium ions are secreted in the distal convoluted tubule and collecting duct and the end result is urine.
 UHI/ CC0
UHI/ CC0
Collecting duct - Little active transport; urine concentration through osmosis.
Loop of Henle - Permeable to H2O and small molecules.
Hormonal control of reabsorption
Reabsorption of some substances is controlled by hormones in the blood stream. For example, blood levels of calcium are controlled by calcitonin, parathyroid hormone and calcitriol – calcitriol directly controls the amount of calcium and phosphate that are reabsorbed or secreted in the kidneys.
Anti-diuretic hormone from the posterior pituitary increases water reabsorption by specifically increasing the permeability of the distal convoluted tubules and the collecting tubules.
Atrial natriuretic peptide secreted by the atria in the heart decreases reabsorption of sodium and water, simultaneously inhibiting secretion of aldosterone and anti-diuretic hormone.
Renal threshold
UHI / CC0
(Click image to toggle animation on/off)
Journey of excess glucose:
Filtrate from glomerulus > Glomerular flitrate > Proximal tubule > Loop of Henle > Distal tubule > Urine
Changes to renal fluis in proximal tubule: Reabsorption of glucose, amino acids, salt and water.
Function of Loop of Henle: To create high osmotic pressure in the kidney medulla.
Changes in renal fluid in distal tubule: Further reabsorption of salts and water and secretion of potassium ions.
Changes in renal fluid collecting duct: Further reabsorption of salts and variable amounts of water and secretion of potassium ions.
The renal threshold of a substance is the kidney’s maximum capacity for reabsorption of a substance. Substances such as glucose are completely reabsorbed unless blood levels are excessively high, when some glucose may remain in the filtrate and appear in the urine (glucosuria).
For example, normal blood glucose levels are between 3.5 to 8 mmol/litre, so blood glucose levels are usually lower than the transport maximum (renal threshold) of 9 mmol/litre and would not usually appear in the urine. Substances such as urea which are not required by the body are secreted into the tubules, transported to the collecting ducts, and excreted out of the body in urine.
Quiz
Now have a go at identifying the functions of the nephron. Match the terms below to the corresponding parts highlighted.
Regulation of blood volume and blood pressure through Anti-Diuretic Hormone
The kidneys are closely involved in blood pressure regulation for the whole body. Blood volume and blood pressure are closely controlled through the absorption and secretion of sodium and water in the kidneys under the control of a hormone called anti-diuretic hormone (ADH), also known as vasopressin.
A diuretic is an agent that increases the rate of urine formation, so anti-diuretic hormone decreases urine formation.
UHI / CC0
(Click image to toggle animation on/off)
Blood water concentration falls > pituitary gland releases more ADH > more water reabsorbed from kidney tubules / small concentration of urine > blood water concentration rises > pituitary gland releases less ADH > less water reabsorbed from kidney tubules / large concentration of dilure urine > and so on...
ADH is secreted from the posterior pituitary in the brain in response to changes in plasma osmolarity (the concentration of solutes in blood). Osmolarity is monitored by brain cells known as an osmoreceptors, and these stimulate secretion of ADH into the blood stream.
ADH binds to cell receptors in the collecting ducts of the kidney, promoting water reabsorption back into the body. In the absence of ADH the collecting ducts are virtually impermeable to water and it flows out as urine. ADH secretion is also stimulated by decreased blood pressure and blood volume, monitored by baroreceptors in the heart and large arteries, though this is not as sensitive as increased osmolarity. Very high levels of ADH can also cause vasoconstriction to elevate blood pressure.
Regulation of blood volume and blood pressure through ADH
UHI / CC0
(Click image to toggle animation on/off)
Filtrate before it becomes urine.
High water volume / high blood pressure
Less ADH is secreted and water remains in the filtrate making urine dilute and plentiful and reducing water volume in the blood.
Low water volume / low blood pressure
More ADH is secreted and water is reabsorbed back in the body. Urine is concentrated and water volume in the blood is increased.
If blood volume is low (i.e. you are dehydrated), blood pressure may also be decreased, and can be elevated by increasing the water volume in the blood.
In response to ADH secretion, water reabsorption back into the body is increased as the walls of the collecting ducts become more permeable to water. Urine is scant and concentrated, blood volume is increased, and blood pressure returns to normal.
If blood volume is high (i.e. you are well hydrated), blood pressure may also be increased, and can be reduced by decreasing the water volume in the blood. In response to reduced ADH secretion, water reabsorption back into the body is decreased in the collecting ducts. Urine is plentiful and dilute as more water is passed from the body, blood volume is decreased, and blood pressure returns to normal.
Quiz
Add the remaining 7 steps into the correct order to illustrate ADH regulation. There are 4 answers which are bogus answers.
Can you spot these and leave them out!?
| 1. | Dehydrated |
| 2. | |
| 3. | |
| 4. | |
| 5. | |
| 6. | |
| 7. | |
| 8. |
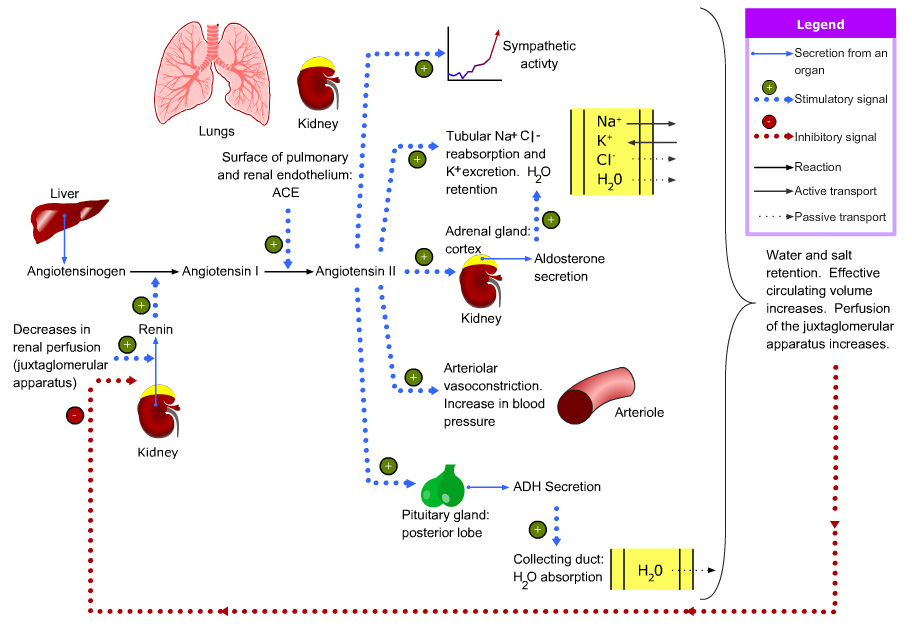
Renin-angiotensin-aldosterone system
Water balance and blood pressure are also controlled through the renin-angiotensin- aldosterone system. When blood volume/blood pressure is low, cells in the afferent arterioles secrete an enzyme called renin, which converts a plasma protein called angiotensinogen (produced by the liver), to be converted to angiotensin 1. Angiotensin 1 is converted into angiotensin 2 by angiotensin converting enzyme (ACE), formed mainly in the lungs and kidneys. Angiotensin 2:
- is a vasoconstrictor and increases blood pressure
- stimulates aldosterone secretion which increases reabsorption of water and salts, increasing water volume and blood pressure
- stimulates ADH secretion, increasing water reabsorption and increasing blood pressure.
Renin, angiotensin 2 and high blood potassium all stimulate aldosterone secretion (from the adrenal cortex), which leads to resorption of water and sodium, hence increasing blood volume and ‘switching off’ renin secretion through a negative feedback mechanism.
 UHI / CC0
UHI / CC0
Regulatory action of atrial natriuretic peptide from the heart
There are a number of factors that stimulate the release of atrial natriuretic peptide (ANP) including levels of blood sodium and angiotensin II. However, primary stimulation is atrial stretching in the heart caused by rising blood pressure. Atrial natriuretic peptide (ANP) decreases blood pressure as follows:
- It relaxes arteriole walls resulting in lower peripheral resistance and blood pressure
- It stimulates water and sodium excretion in the kidneys through a number of pathways
- It reduces aldosterone and renin secretion, causing a drop in the reabsorption of water and sodium ions from kidney tubules
 .jpg?1612890706130)
This increases urine flow, reduces internal water volume, and decreases blood pressure.
Micturition reflex
When the bladder is half-full, stretch receptors in the wall are stimulated. In an infant this initiates a spinal reflex which causes the bladder wall to contract, both sphincters relax and so urine leaves via the urethra. We learn to control our bladders as children by controlling the sphincter muscles.
In adults, sensory information is sent to the brain in addition to the stretch reflex from the bladder wall creating an awareness of the need to pass urine. Contraction of the external urethral sphincter and muscles of the pelvic floor inhibit micturition for a limited period.
Micturition occurs in adults when the detrusor muscle contracts and there is reflex relaxation of the internal urethral sphincter together with voluntary relaxation of the external sphincter. The detrusor muscle is a mass of interlacing smooth muscle fibres and elastic tissue arranged in three layers. When it contracts it empties the bladder.
The composition of urine
Substances in the glomerular filtrate – the substances that have filtered out of the blood stream in the glomerulus – that have not been reabsorbed from the proximal and distal tubules and Loop of Henle eventually form urine. The filtrate is collected in the collecting ducts, emptied into the calyces, propelled down the ureters and stored in the bladder.
| The composition of urine: | |
|---|---|
| Water | 96% |
| Urea | 2% |
|
Uric acid |
2% |
Test your knowledge
Now it's time to test your knowledge of the urinary system. There are 10 questions to complete.
You might want to take some time to read your notes, draw diagrams before you test yourself!
Summary
You have completed your study of the urinary system.
You should now have a good knowledge and understanding of the anatomy and physiology of the urinary system. You should be able to:
- Describe the structure of the urinary system
- Explain the functions of the kidneys
- Describe kidney microstructure
- Explain the formation of urine process
- Explain the regulation of water volume & blood pressure
- Describe micturition
If you think that your knowledge or understanding of any section of the urinary system could be improved further, go back to the relevant sections and work through them again, taking time to make notes and complete the activities.



.png?1612456456666)
 UHI / CC0
UHI / CC0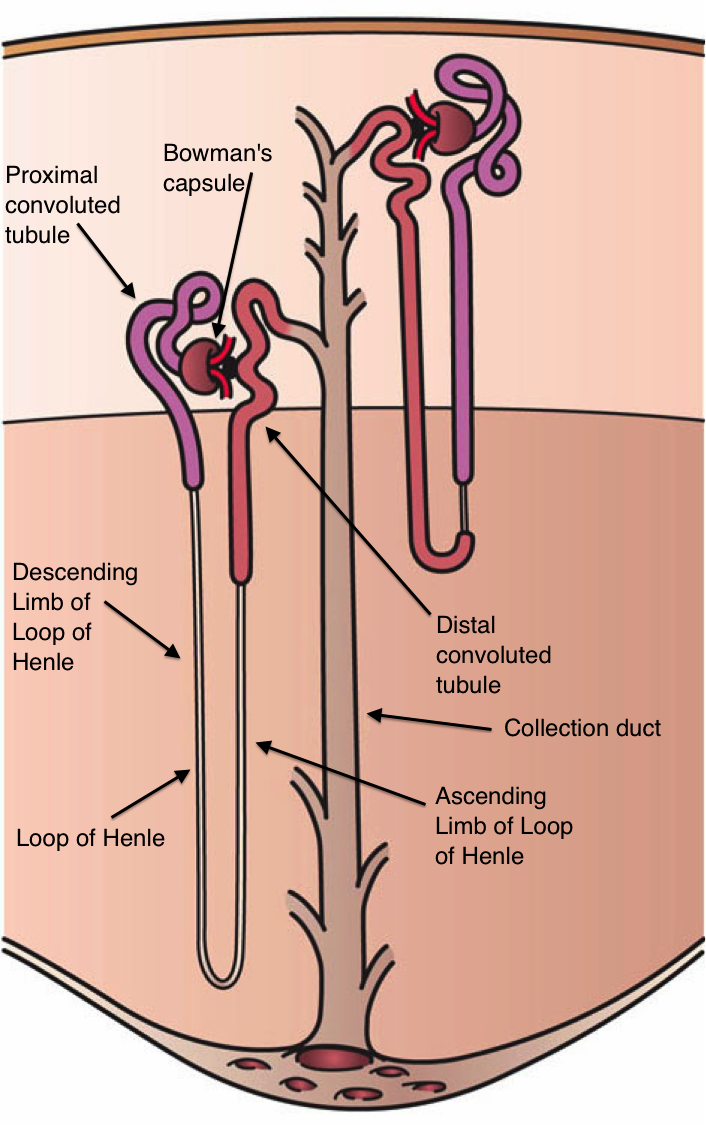
.png?1612891298552)