Introduction
You might work through this system over several weeks, days or hours, but to enhance your learning and enjoyment make sure you break it up into bite-size chunks.
Here are the sections of the endocrine system:
As you study the endocrine system you will learn about:
- Endocrine hormones and target cells
- Negative and positive feedback mechanisms
- The hypothalamus
- Control of the endocrine system
- The pituitary gland
- The thyroid gland
- The adrenal glands
- The pancreas
- Gonadotrophin releasing hormone.
Make notes as you study each section, and interact fully with the activities – watch the animations and complete the quizzes.
Take a break at the end of each section– resting your eyes from the computer screen, getting some fresh air or taking a coffee break will improve your ability to focus on your study and take in information.
Give yourself time to think about what you have learned, and time to absorb and understand it.
UHI / CC0
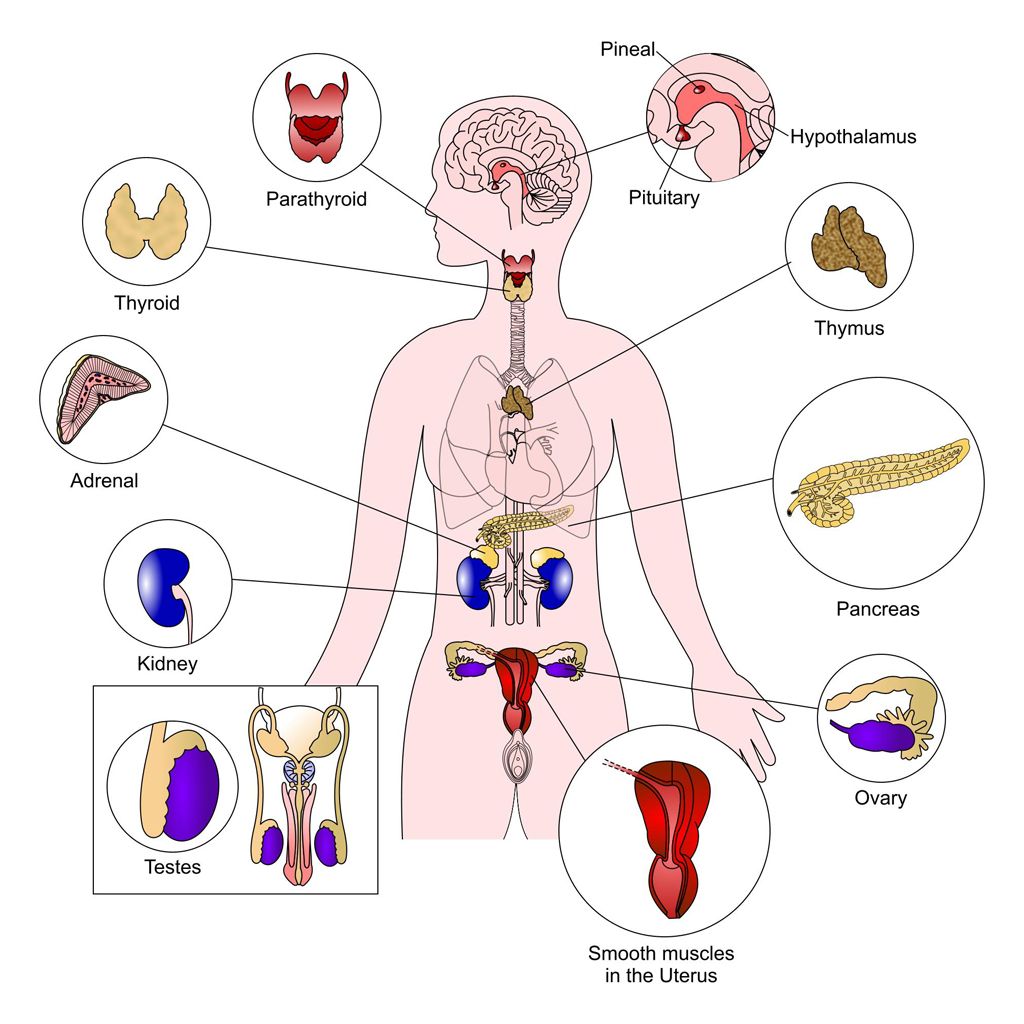
The endocrine system
Together with the autonomic nervous system, the endocrine system helps to maintain balance (homeostasis) within the body. Whereas the nervous system is usually concerned with rapid changes, the endocrine system often creates slower or more precise adjustments in the body.
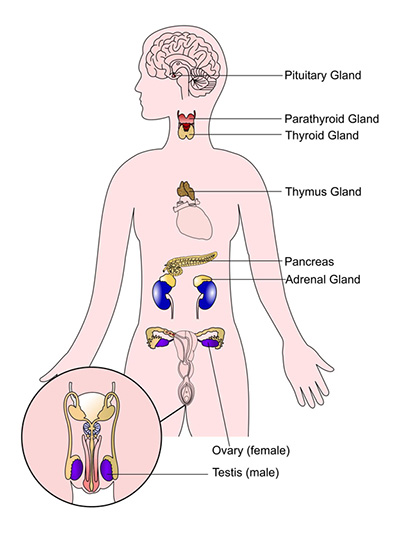
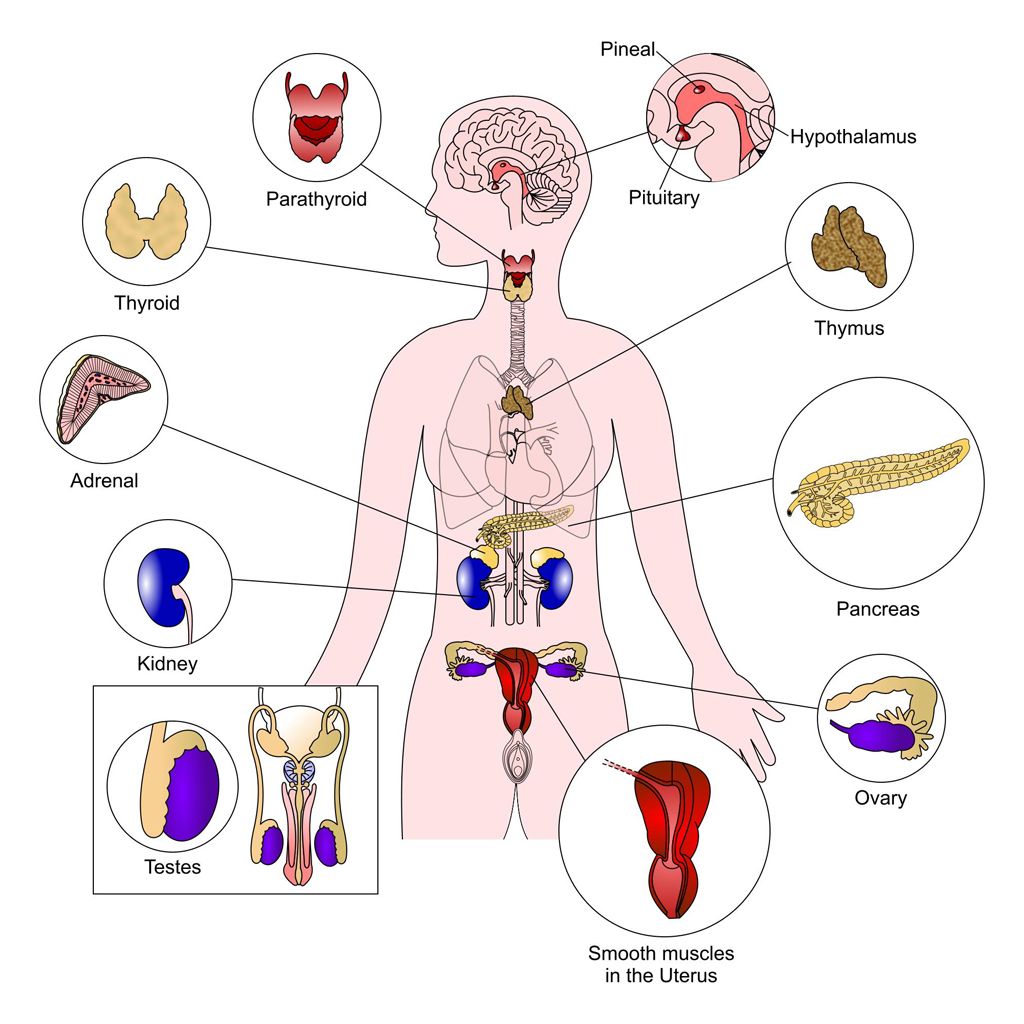
The endocrine system is composed of several endocrine organs or glands which secrete a series of chemical messengers known as hormones. The endocrine glands are surrounded by a dense capillary network allowing easy distribution of hormones into the blood stream. These hormones regulate cell function by targeting specific groups of cells, tissues or organs.
Together with the autonomic nervous system, the endocrine system helps to maintain balance (homeostasis) within the body. Whereas the nervous system is usually concerned with rapid changes, the endocrine system often creates slower or more precise adjustments in the body.
The endocrine system is composed of several endocrine organs or glands which secrete a series of chemical messengers known as hormones. The endocrine glands are surrounded by a dense capillary network allowing easy distribution of hormones into the blood stream. These hormones regulate cell function by targeting specific groups of cells, tissues or organs.
Following stimulation from the nervous system or in response to hormone levels, endocrine hormones are released into the blood stream and circulated around the body
Endocrine hormones and target cells
Hormones only affect their target cells as each hormone binds to receptor molecules on/in the target cells. For example, insulin can target muscle and liver cells as these cells have insulin receptors on the outside of the cell membrane, but would have no effect on uterine cells as these cells do not have insulin receptors.
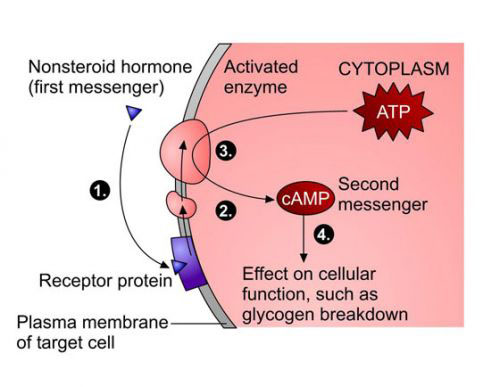
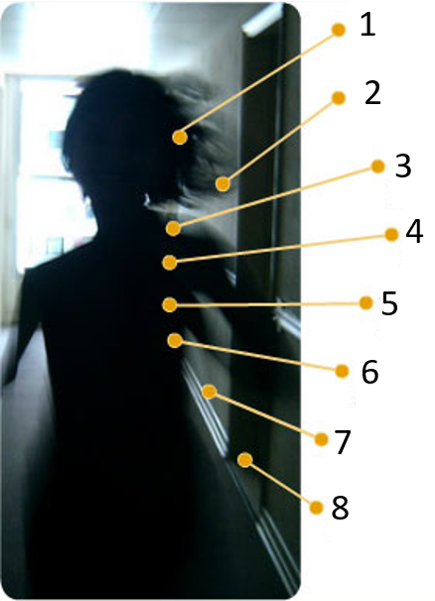
Different types of endocrine hormones have different mechanisms for entering a cell. Cell receptors for peptide hormones are located on the cell membrane and are like a ‘gate’ (image 1); receptors for lipid-based hormones are inside the cell (image 2).
UHI / CC0
- Nonsteroid hormone (first messenger)
- Plasma membrane of target cell
- Receptor protein
- Cytoplasm
- Activated enzyme
- ATP
- cAMP Second messenger
- Effect on cellular function, such as glycogen breakdown
Peptide hormones include:
- adrenaline
- noradrenaline
- insulin
- glucagon.
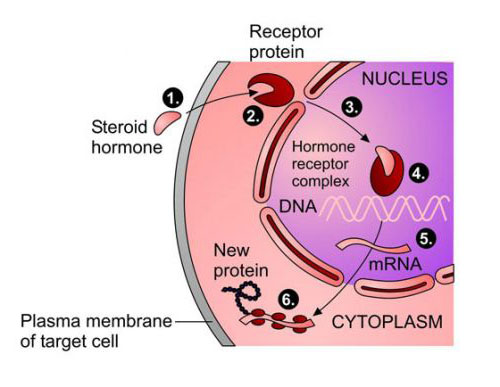
UHI / CC0
- Steroid hormone
- Plasma membrane of target cell
- Cytoplasm
- Receptor protein
- Nucleus
- Hormone receptor complex
- DNA
- mRNA
- Cytoplasm
- New protein
Lipid-based hormones include the:
- glucocorticoids
- mineralocorticoids (steroids)
- thyroid hormones.
Once a hormone has bound on to its target cell, it catalyses a chemical or metabolic reaction within the cell.
Hormonal control within the body
Blood levels of hormones can be quite variable, and are largely self-regulating.
If hormone levels are low, this is called hyposecretion; if hormone levels are too high, this is known as hypersecretion. Either of these conditions may be due to a problem with the feedback mechanism or another health condition that may be affecting hormonal secretion.
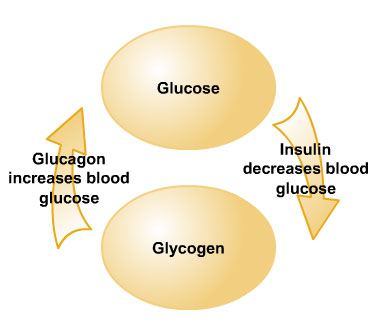
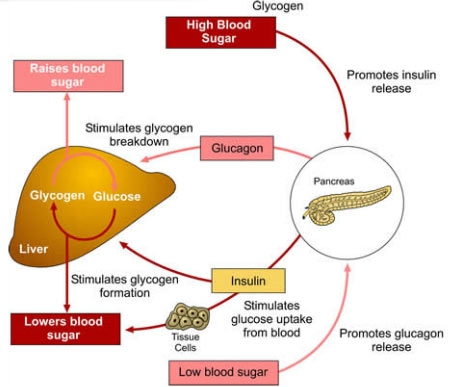
Some hormones come in antagonistic pairs, having opposite effects upon their target cells. For example, insulin and glucagon have opposing effects upon blood glucose levels.
Negative and positive feedback mechanisms
Hormonal regulation usually depends on negative or positive feedback mechanisms.
Negative feedback mechanism
Negative feedback mechanisms (also known as loops) work when high levels of the hormone in question turns off its own secretion. This may be controlled via the hypothalamus or pituitary gland (steroid and thyroid hormones, for example), or controlled by blood levels of the hormone itself.
Positive feedback mechanism
A positive feedback mechanism results in amplification of the stimulus and increased release of the hormone involved until a particular process is complete and the stimulus ceases. One example of this is the release of oxytocin during labour.
The hypothalamus and pituitary glands
The hypothalamus is part of the brain and not an endocrine organ itself, but it controls the pituitary gland and has an indirect effect upon most endocrine organs. The hypothalamus and pituitary act as one unit, regulating the activity of most endocrine glands.
The hypothalamus secretes releasing or inhibiting hormones into the pituitary portal system, a blood stream which flows directly to the pituitary from the hypothalamus. Secretions of the anterior pituitary can be stimulated or inhibited by the production of hormones from the hypothalamus.
These hormones released by the hypothalamus and stimulating the pituitary are called releasing hormones.
UHI / CC0
Control of the endocrine system
For secretion of many endocrine hormones, low levels of a hormone in the blood stream stimulates secretion of the appropriate releasing hormone from the hypothalamus, which travels to the pituitary gland, stimulating release of a trophic hormone which travels in the bloodstream to its target endocrine organ.
A trophic hormone travels to another endocrine organ to stimulate release of the hormone that was needed in the blood stream in the first place).
After the release and resultant elevated blood levels of this hormone, secretion of the releasing hormone from the hypothalamus will be inhibited, or an inhibiting hormone released from the hypothalamus. This series of events describes a typical negative feedback mechanism.
UHI / CC0
(Click image to toggle animation on/off)
- Neurosecretory cells of the hypothalamus
- Pituitary portal system
- Anterior pituitary
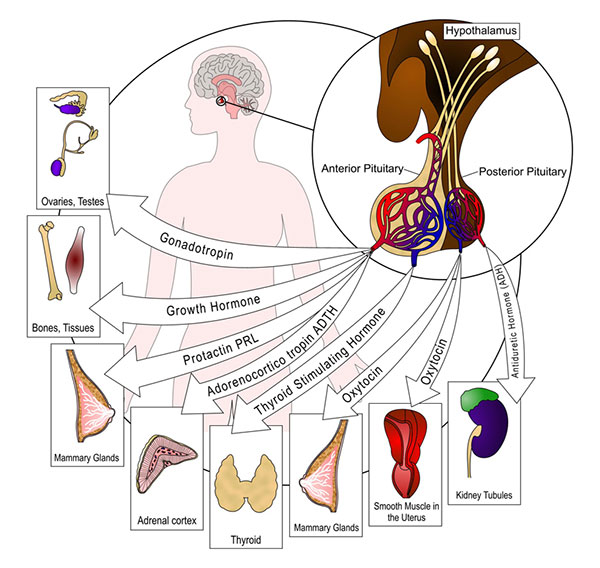
Hormones of the anterior pituitary gland
The pituitary gland is the link between the nervous system and the endocrine system. It regulates so many other hormone producing tissues that it is called the ‘master gland’, and is divided, both structurally and functionally, into the anterior and posterior pituitary.
Some hormones secreted from the anterior pituitary have a direct effect upon target tissues. Others regulate the hormone output of other endocrine glands. Hormones produced by the anterior pituitary are:
- Growth hormone
- Prolactin
- Follicle stimulating hormone FSH)
- Luteinising hormone (LH)
- Thyroid stimulating hormone
- Adrenocorticotrophic hormone (ACTH).
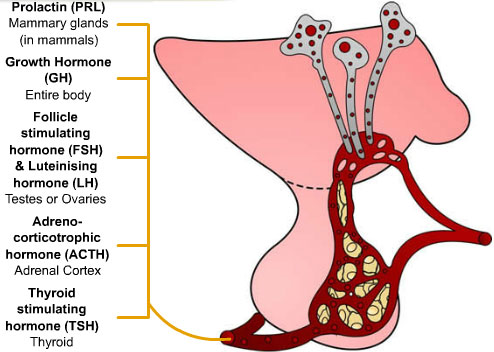
UHI / CC0
- Prolactin (PRL): Mammary glands (in mammals)
- Growth hormone (GH): Entire body
- Follicle stimulating hormone (FSH) and luteinising hormone (LH): Testes or ovaries
- Adrenocorticotrophic hormone (ACTH): Adrenal cortex
- Thyroid stimulating hormone (TSH): Thyroid
Quiz
Click on the statements that are True below.
Growth hormone
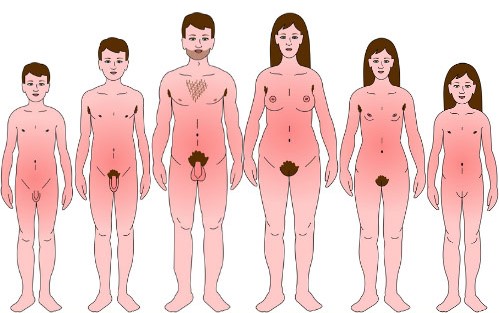
Growth Hormone (GH) is produced throughout life, although the greatest impact is on cells of the skeletal and muscle tissue in children and adolescents. After puberty it is largely involved in maintenance, with output increasing during sleep and exercise.
Release of growth hormone is stimulated by Growth Hormone Releasing Hormone (GHRH) (somatotropin) from the hypothalamus. Its secretion is inhibited by Growth Hormone Release Inhibiting Hormone (GHRIH) (somatostatin) via a negative feedback mechanism.
Growth hormone stimulates growth, regulates metabolism, stimulates protein synthesis, break down of adipose tissue, and increases blood glucose levels by stimulating conversion of glycogen to glucose.
UHI / CC0
(Click image to toggle animation on/off)
Growth hormone ensures an ongoing fuel supply as well as facilitating growth. Hyposecretion (under production) of GH causes bones to grow very slowly and the epiphyseal growth plates may seal before normal height is achieved. This is known as pituitary dwarfism. Many other body organs also do not grow to full adult size. This can be treated by the use of synthetic GH given under medical supervision during childhood years while the epiphyseal plates are still open.
In children, overproduction (hypersecretion) of HGH leads to gigantism due to the rapid increase in bone length. Hypersecretion in adults leads to a condition called acromegaly. The bones of the hands, feet and lower jaw overgrow and soft tissues such as the tongue and nose may also thicken. At puberty, the growth spurt seen in teenagers occurs as oestrogen and testosterone stimulate the secretion of GH that stimulates growth.
Growth hormone stimulates growth
UHI / CC0
Prolactin
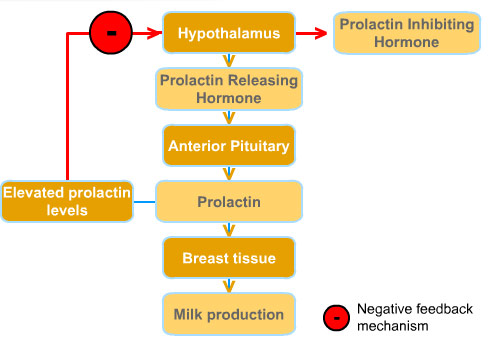
Release of prolactin is stimulated by Prolactin Releasing Hormone (PRH), and lowered by Prolactin Inhibiting Hormone (PIH) (dopamine), from the hypothalamus when blood levels are elevated.
Increased blood levels of prolactin inhibit further release of prolactin via a negative feedback mechanism. Suckling stimulates prolactin secretion and lactation. This high blood level of prolactin after birth reduces the incidence of conception during lactation. Prolactin secretion is elevated during sleep and during emotional stress.
Prolactin stimulates development of mammary glands during pregnancy and stimulates milk production.
UHI / CC0
- Hypothalamus
- Prolactin releasing hormone
- Anterior pituitary
- Prolactin
- Breast tissue
- Milk production
Negative feedback mechanism:
- Elevated prolactin levels
- Hypothalamus
- Prolactin inhibiting hormone
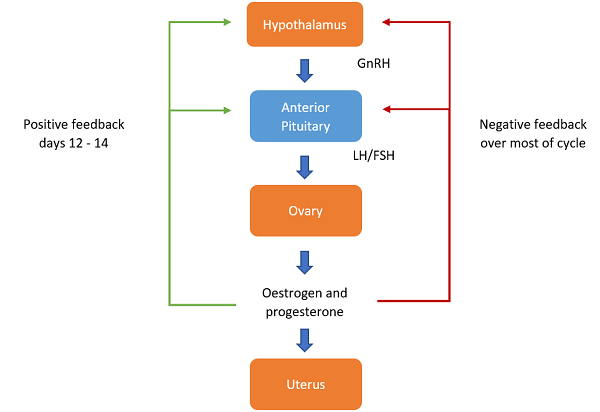
The gonadotrophins
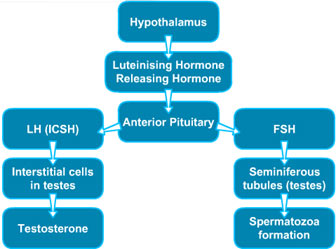
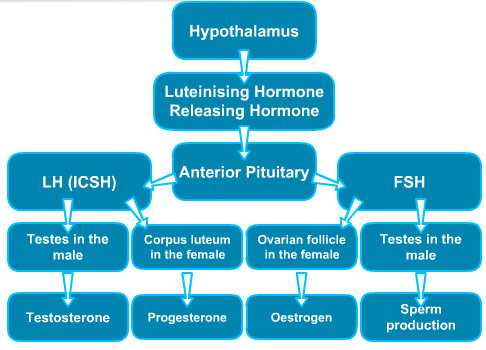
After puberty Luteinising Hormone (LH) and Follicle Stimulating Hormone (FSH) are secreted by the anterior pituitary in response to Luteinising Hormone Releasing Hormone (LHRH), also known as Gonadotrophin Releasing Hormone (GnRH) secreted by the hypothalamus.
Follicle stimulating hormone (FSH) stimulates production of sperm and testosterone secretion in males, and stimulates follicular growth in the ovaries.
Luteinising hormone (LH) stimulates the interstitial cells in the testes to produce testosterone, and in the female it triggers ovulation and stimulates development of the corpus luteum.
LH and FSH also affect the secretion of the sex hormones oestrogen, progesterone and testosterone, via both negative and positive feedback mechanisms.
UHI / CC0
The thyroid hormones
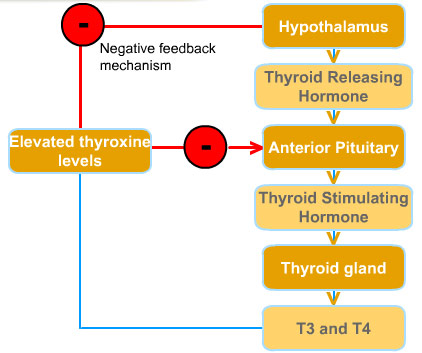
Release of Thyroid Stimulating Hormone (TSH) from the anterior pituitary is stimulated Hormone (TRH) from the hypothalamus.
TSH secretion is inhibited by a negative feedback loop when blood levels of thyroxin (T4) are high.
The trophic Thyroid Stimulating Hormone stimulates production of thyroxin (T4) and tri-iodothyronine (T3) from the thyroid gland. These hormones regulate the metabolic rate of the body, determining the rate of cellular metabolism of all cells, the rate at which we utilize energy (calories), and the body heat generated.
UHI / CC0
- Hypothalamus
- Thyroid releasing hormone
- Anterior pituitary
- Thyroid stimulating hormone
- Thyroid gland
- T3 and T4
Negative feedback mechanism:
- Hypothalamus
- Elevated thyroxine levels
- Anterior pituitary
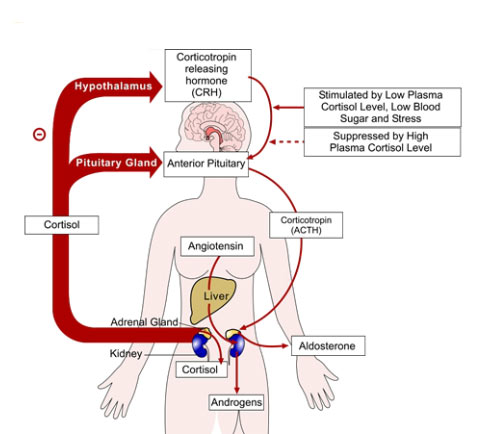
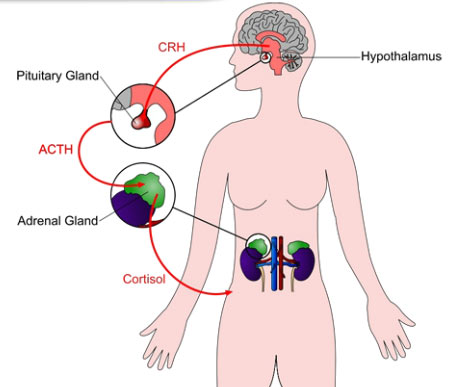
Adrenocorticotropic hormone
Synthesis and release of Adrenocorticotropic hormone (ACTH) (also known as corticotrophin) from the anterior pituitary gland is stimulated by Corticotrophin Releasing Hormone (CRH) from the hypothalamus.
ACTH travels to the adrenal glands and stimulates synthesis and secretion of cortisol from the cortex of the adrenal glands. It also increases the concentration of cholesterol and steroids in the adrenal cortex.
Elevated levels of blood cortisol ‘switch off’ secretion of ACTH and CRH in a negative feedback loop.
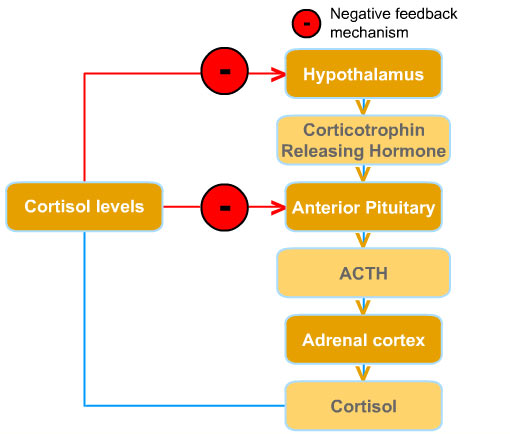
UHI / CC0
- Hypothalamus
- Corticotrophin releasing hormone
- Anterior pituitary
- ACTH
- Adrenal cortex
- Cortisol
Negative feedback mechanism:
- Cortisol levels
- Hypothalamus
- Anterior pituitary
Quiz
Hormones of the posterior pituitary gland
The posterior pituitary is not really endocrine tissue as it stores, rather than releases, hormones. Oxytocin and anti-diuretic hormone (ADH), also known as vasopressin, are synthesised in the hypothalamus and stored in the posterior pituitary gland. These hormones act on non-endocrine tissues, and their release is stimulated by nervous impulses from the hypothalamus.
Oxytocin is responsible for the dilation of the cervix during birth and causes contractions during labour. As a child breast feeds, stimulation of the pressure receptors in the nipple feeds back to the hypothalamus causing release of more oxytocin. This in turn causes further contraction of the uterus, sealing blood vessels that may have been torn during the birth process. Oxytocin also increases milk production for breast feeding.
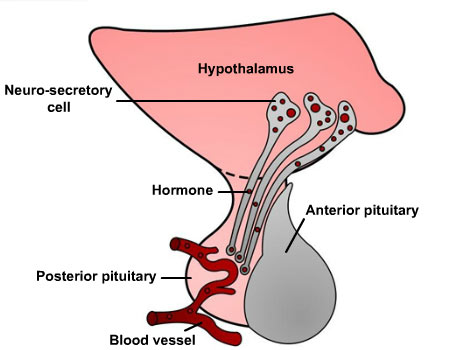
UHI / CC0
- Hypothalamus
- Neuro-secretory cell
- Hormone
- Posterior pituitary
- Blood vessel
- Anterior pituitary
Anti-diuretic hormone
Blood osmolarity is continually monitored by osmosreceptors in the hypothalamus, and anti-diuretic hormone (ADH) is released into the blood stream when the blood is too concentrated (hypertonic). A diuretic is an agent that increases the rate of urine formation, so anti- diuretic hormone decreases urine formation.
As ADH filters through the kidney, it causes more water to be re-absorbed back into the body from the urine that has been produced. This reduces blood concentration by increasing water volume of the blood, and also leads to a rise in blood pressure. The resulting higher water volume and reduced blood concentration ‘switches off’ ADH secretion via a negative feedback loop. ADH also causes vasoconstriction of arterioles throughout the body which also increases blood pressure.
UHI / CC0
(Click image to toggle animation on/off)
Cycle:
- blood water concentration falls
- pituitary gland releases more ADH
- more water reabsorbed from kidney tubules, small concentration of urine
- blood water concentration rises
- pituitary gland releases less ADH
- less water reabsorbed from kidney tubules, large concentration of dilute urine
- (back to beginning)
Quiz
The thyroid gland
The thyroid gland is located in the neck. It consists of two lobes held together by a band of tissue called the isthmus. The thyroid gland consists of cells called follicles which secrete hormones T3 (tri-iodothyronine) and T4 (thyroxine) into the internal spaces of the follicles. From here, the hormones are released into the blood stream.
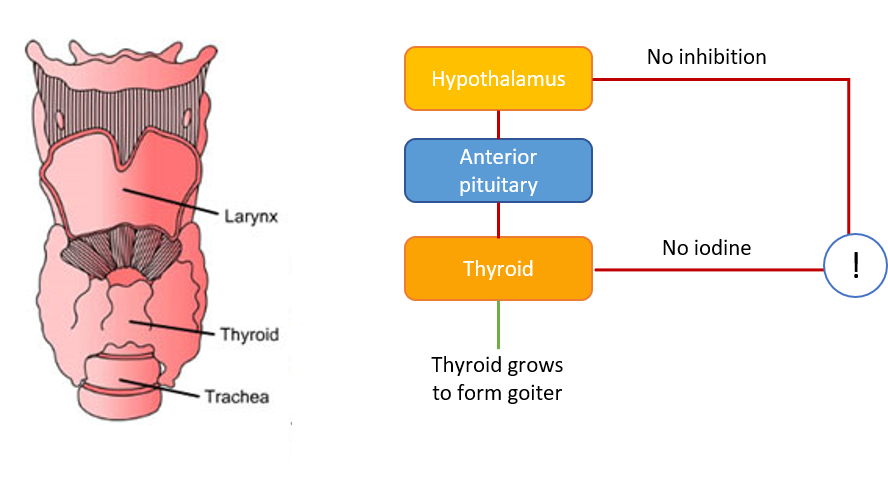
UHI / CC0
Larynx
Thyroid
Trachea
- Hypothalamus: no inhibition
- Anterior pituitary
- Thyroid: no iodine
- Thyroid grows to form goiter
Iodine in our diet forms a part of the molecular structure of these hormones, 3 iodine atoms in T3, 4 iodine atoms in T4 (hence the names T3 and T4). An iodine deficiency causes excess TSH to be secreted and the thyroid gland enlarges (called a goitre) in attempt to trawl more iodine from the blood system. However, only small amounts of iodine are needed, and it is present in many different foods.
Thyroxin and tri-iodothyronine
Secretion of Thyroid Stimulating Hormone (TSH) is increased by exercise, malnutrition, stress, low blood glucose and sleep. All cells in the body are targeted by T3 and T4 hormones, and output is regulated by a negative feedback loop as high levels of thyroid hormones decrease TSH secretion.
Thyroid hormones control our metabolic rate - the number of calories we use up during a day. More thyroid hormone is produced during winter than in summer: the hypothalamus senses a reduction in body temperature with exposure to cold weather and releases more Thyroid Releasing Hormone. This increases Thyroid Stimulating Hormone output from the pituitary, causing an rise in T3 and T4 output.
Thyroid hormones increase metabolic rate and heat production. They also increase heart rate and cardiac output, and are essential for growth and development.
Calcitonin
The thyroid gland is also responsible for the production of another hormone called calcitonin. Together with secretions from the parathyroid glands, this hormone regulates blood calcium levels. Calcitonin stimulates osteoblast activity, increasing the amount of calcium deposited in bone, resulting in lower blood calcium levels. Calcitonin inhibits osteoclast activity (prevents reabsorption of calcium and phosphates in the kidney tubules, so these minerals are lost in the urine rather than being reabsorbed back into the blood stream.
The concentration of calcium in extracellular fluid is the main factor controlling calcitonin release. High blood calcium levels stimulate calcitonin release, and calcitonin production falls when plasma calcium levels fall below normal.
UHI / CC0
(Click image to toggle animation on/off)
- High concentration of calcium in blood
- Release of calcitonin from thyroid gland
- Reduced concentration of calcium in blood
The parathyroid glands and parathyroid hormone
Parathyroid hormone is produced by the parathyroid glands located on the thyroid gland. The major targets for this hormone are the bone and the kidneys. Parathyroid hormone increases blood calcium levels by:
- stimulating osteoclasts to break down bone releasing calcium into the blood stream'
- stimulating kidney tubules to increase reabsorption of calcium from urine back into the blood stream, increasing blood calcium levels.
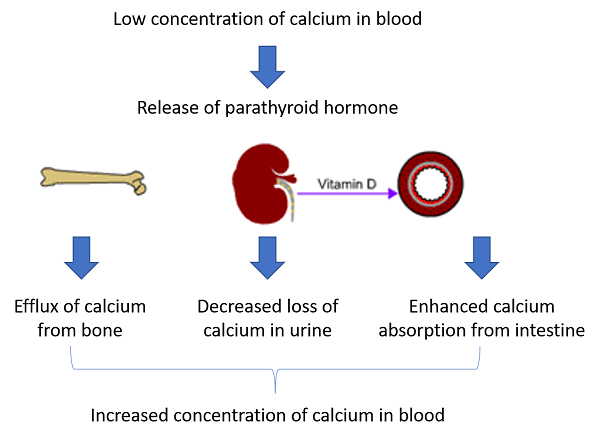
UHI / CC0
- Low concentration of calcium in blood
- Release of parathyroid hormone
- Efflux of calcium from bone
- Decreased loss of calcium in urine
- Enhanced absorption of calcium from intestine
- Increased concentration of calcium in blood
Calcitriol
Parathyroid hormone also increases calcium absorption indirectly by travelling to the kidneys and stimulating the production of calcitriol.
Calcitriol travels in the blood stream to the intestines, where it increases production of a calcium-binding protein in the epithelial cells of the gut lining, increasing calcium absorption from food eaten into the blood stream.
Quiz
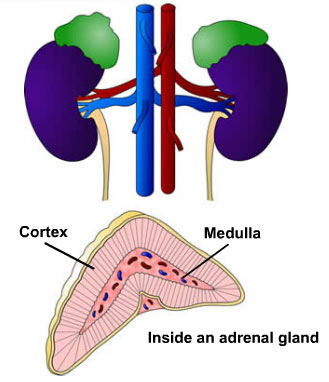
The adrenal glands – glucocorticoids, mineralocorticoids and catecholamines
The two adrenal glands are located at the top of the kidneys, and each adrenal gland consists of an outer cortex and an inner medulla.
The outer cortex secretes several types of steroid hormones including glucocorticoids and mineralocorticoids.
The inner medulla is stimulated by the sympathetic nervous system, and produces the catecholamines adrenaline (epinephrine) and noradrenaline (norepinephrine).
Adrenaline and noradrenaline
Adrenaline and noradrenaline (also known as epinephrine and norepinephrine) are known as the catecholamines and, together, they have very similar actions and create the ‘fight or flight’ response.
The fight or flight response
- Senses and perception sharpen. Time may appear to 'slow down'.
- Blood flow to muscles increases. They become tense and ready for action.
- Heart beats faster increasing blood pressure and preparing us for peak exertion.
- We breathe more rapidly oxygenating the blood ready to fight or flee.
- We want to urinate or may empty our bowels. This makes us lighter so we can run faster.
- Digestion stops. Blood is diverted from the gut to the arms and legs.
- Substances are released that make the blood 'stickier' so we will lose less blood if injured.
- We start to sweat profusely, cooling us for exertion and making it less easy to be grabbed.
Noradrenaline acts as a neurotransmitter (a chemical which enables nervous stimuli to pass across synapse in the nervous system). Both of these hormones are released during stimulation of the sympathetic nervous system. Secretion of adrenaline and noradrenaline is induced by exercise, hypoglycaemia (low blood sugar), haemorrhage, emotional distress, stressful situations and drinking caffeinated drinks.
The effects of adrenaline and noradrenaline
These hormones have a similar effect on organs as direct stimulation by sympathetic nerves, and are released when immediate energy and fast responses are required, although their effect is longer lasting than stimulation from the nervous system. The effects of catecholamine release are:
- increased heart rate
- increased blood pressure
- general vasoconstriction
- blood diversion and vasodilation in areas which need it
- bronchiole dilation to increase air intake increased glycogen and fat breakdown for energy
- increased metabolic rate
- increased oxygen consumption
- heat production
- dilation of the pupils
- inhibition of non-essential processes such as digestion
UHI / CC0
Hormones from the adrenal cortex
Many different steroid-based hormones are produced in the adrenal cortex but there are two main classes – the glucocorticoids and the mineralocorticoids.
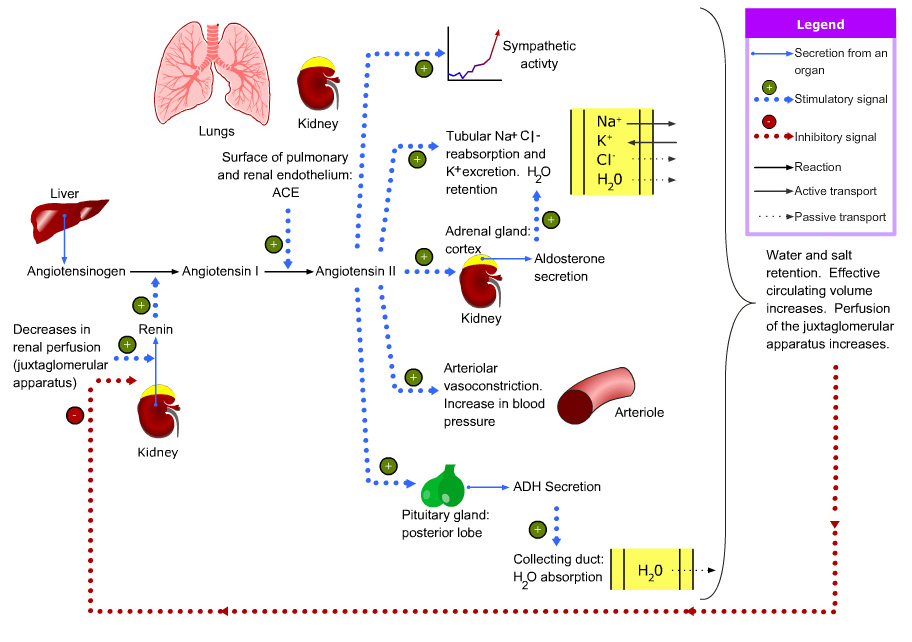
The main glucocorticoid is cortisol, and it regulates carbohydrate metabolism. The main mineralocorticoid is aldosterone, which is involved in the homeostatic internal balance of sodium ions (Na+), potassium ions (K+) and water via the kidneys.
The adrenal cortex also produces some sex steroids known as androgens.
Glucocorticoids - cortisol
Cortisol secretion is highest in the morning and lowest at night. Every cell in the body has glucocorticoid receptors so cortisol has a wide range of effects in the body. The most important effects are on carbohydrate metabolism and immune function. Glucocorticoids such as hydrocortisone are often prescribed for their anti-inflammatory and immunosuppressive properties.
The central nervous system is ultimately responsible for glucocorticoid responses via stimulation of the hypothalamus, providing an example of close integration between the nervous and endocrine systems. Mental or physical stress raises CRH levels from the hypothalamus, increasing glucocorticoid levels.
Effects of glucocorticoids (cortisol)
During stressful times the body requires instant energy in the form of glucose, so cortisol facilitates this in a number of ways.
Stimulation of gluconeogenesis (formation of glucose) involving the production of glucose from non-carbohydrate sources such as amino acids
Stimulation of lipolysis in adipose tissue – fatty acids are released and used by muscle cells for energy, sparing glucose use
Inhibition of glucose uptake in muscle and adipose tissue, which means that blood glucose levels stay elevated
Breakdown of body proteins to free amino acids for gluconeogenesis.
Mineralocorticoids - aldosterone
Aldosterone plays a critical role in regulating mineral concentrations in extracellular fluids, particularly sodium and potassium. Lack of mineralocorticoids rapidly leads to life-threatening abnormalities in electrolyte and fluid balance. The kidney tubules are the targets for aldosterone, where it influences the reabsorption and exchange of sodium and potassium ions. It increases blood and water volume in the kidneys in a number of ways.
- Reducing sodium ion loss in urine
- This increases osmotic pressure of the blood and increases water reabsorption
- Increased potassium ion
Aldosterone also reduces sweat and saliva production, leading to a conservation of body sodium, and increases water absorption in the colon.
UHI / CC0
Control of aldosterone output is very complicated as it is influenced by other factors that impact on and regulate fluid and electrolyte balance. If renal (kidney) blood volume falls, the renin-angiotensin-aldosterone system is triggered, resulting in aldosterone secretion and an increase in blood volume and increased blood pressure.
Atrial naturetic hormone, secreted by the atria of the heart, a high blood sodium level and potassium deficiency all reduce aldosterone secretion.
Aldosterone deficiency can occur by itself but is more common as a side effect of Addison’s disease. Without treatment, a lack of aldosterone produces electrolyte imbalance leading to hypotension and eventual death.
Immediate & longer lasting adrenal effects
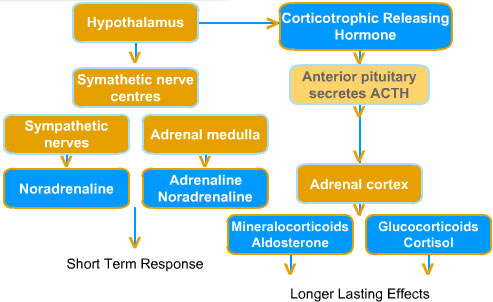
Short term response:
High heart rate
High blood pressure
Bronchioles dilate
High blood glucose
Low digestion levels
Longer lasting effects:
High fat, protein and glucose use
Low immune response
Low inflammation
Increased fuel availability
Reduced inflammatory response
Quiz
Endocrine organs
UHI / CC0
UHI / CC0
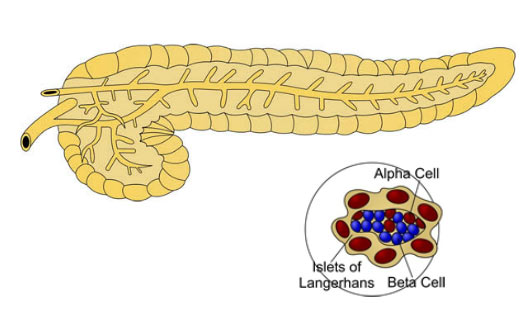
The pancreas
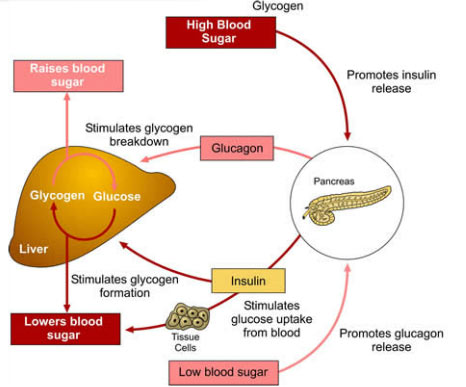
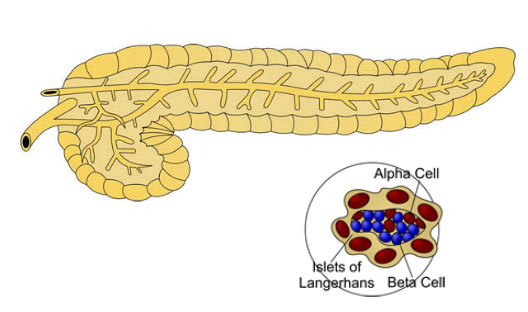
The pancreas is located behind the stomach and consists of two types of tissue: exocrine tissue (which makes digestive enzymes which are emptied into the small intestine), and endocrine tissue, which produces hormones to regulate blood glucose levels.
The endocrine tissue is made up of small clusters of cells called the Islets of Langerhans. There are 3 types of islet cells:
- alpha (α) cells produce the hormone glucagon which raises blood sugar levels
- beta (β) cells produce the hormone insulin which lowers blood glucose levels
- delta (Δ) cells produce somatostatin (also called growth hormone release inhibiting hormone), which inhibits production of insulin and glucagon and slows nutrient absorption in the gut.
Insulin
Insulin increases the rate at which glucose can pass through cell membranes. Increased blood concentrations of amino acids and fatty acids also promote insulin secretion.
Insulin reduces blood glucose in a number of ways.
- It increases cellular uptake of glucose
- It increases glycogenesis (conversion of glucose to glycogen in liver and muscle cells)
- It increases cellular uptake of amino acids, increasing protein synthesis
- It inhibits gluconeogenesis (formation of new glucose from amino acids)
- It decreases lipolysis (use of fat for fuel) so that excess glucose
- It increases fat storage as fatty acids are stored instead of used as fuel
- It inhibits conversion of glycogen to glucose (glycogenolysis) as glucose levels are already elevated.
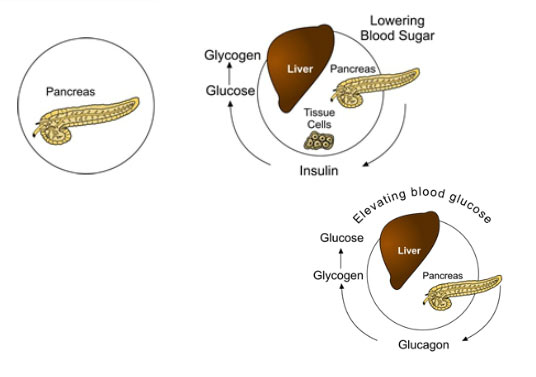
UHI / CC0
Lowering blood sugar:
- Pancreas
- Tissue cells: insulin
- Liver: glucose to glycogen
Elevating blood sugar:
- Pancreas
- Glucagon
- Liver: glycogen to glucose
Control of blood glucose levels
After a carbohydrate rich meal, blood glucose levels increase, and insulin is released in response. All cells require fuel to function, and glucose is a preferred energy source. Without insulin, body cells cannot absorb glucose and switch to using alternative fuels like fatty acids for energy, although these are only partially broken down in the absence of glucose. The brain also requires glucose to function and is the only tissue that does not require insulin for efficient uptake of glucose.
Glucose is also stored as glycogen in the liver and muscles. This is converted back into glucose by the hormone glucagon when blood glucose levels drop again. When liver glycogen reserves are full, additional glucose converted into fatty acids and stored as adipose tissue (fat). Insulin is an anabolic hormone, building protein, fat and glycogen reserves.
Insulin receptors
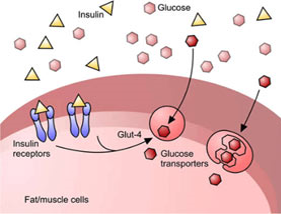
UHI / CC0
Insulin, Glucose
Fat/muscle cells:
- Insulin receptors
- Glut-4
- Glucose transporters
The number and functionality of insulin receptors is affected by insulin levels, exercise and food intake. Exposure to increased levels of insulin following a diet rich in sugary or refined carbohydrates can decrease receptor concentration leading to insulin resistance, where the cell receptors stop responding to insulin and fail to allow glucose entry into the cell. This causes the blood glucose level to remain elevated (hyperglycaemia) and reduces energy availability for cells. Insulin levels may also be high (hyperinsulinaemia). Hyperglycaemia also causes further complications such as glycosuria (glucose in the urine) and can lead to Type 2 diabetes.
Diminished glucose uptake:
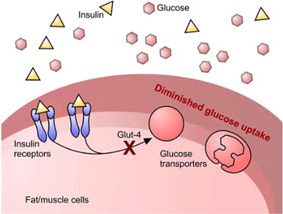
UHI / CC0
Insulin, Glucose
Fat/muscle cells:
- Insulin receptors
- Diminished glucose uptake
- Glut-4
- Glucose transporters
Exposure to decreased insulin levels increases insulin receptor sensitivity as the cells need to maximise uptake of glucose and other energy sources. The number of receptors increases in starvation and decreases in obesity.
Glucagon
This hormone is released from the pancreatic beta cells in response to low blood levels of glucose. Glucagon prompts the following reactions:
- Glycogenolysis (conversion of glycogen to glucose)
- Gluconeogenesis (production of new glucose from amino acids).
Elevated blood levels of amino acids after consumption of a protein-rich meal also stimulate glucagon secretion. Glucagon increases conversion of excess glucogenic amino acids (may be converted into glucose) into glucose. Exercise also stimulates glucagon secretion due to the exercise-induced depletion of glucose in the blood stream.
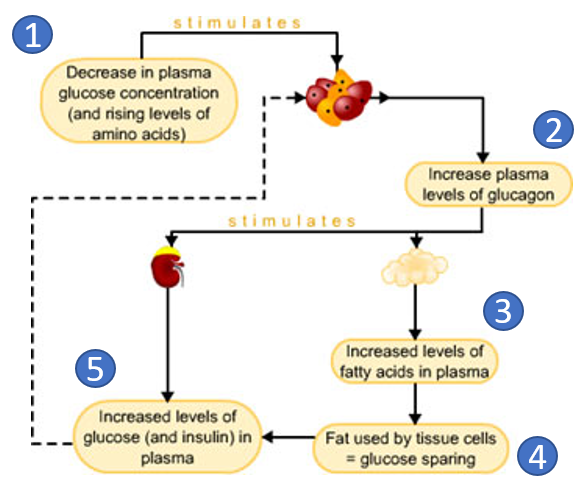
UHI / CC0
- Decrease in plasma glucose concentration (and rising levels of amino acids)
- Increase plasma levels of glucagon
- Increased levels of fatty acids in plasma
- Fat used by tissue cells = glucose sparing
- Increased levels of glucose (and insulin) in plasma
Quiz
Luteinising hormone and follicle stimulating hormone
Luteinising hormone and follicle stimulating hormone in the female
The hypothalamus releases Gonadotrophin Releasing Hormone (GnRH), also known as Luteinising Hormone Releasing Hormone. This stimulates the release of Follicle Stimulating Hormone (FSH) and Luteinising Hormone (LH) from the anterior pituitary gland. The target endocrine gland in females is the ovary, and in the male, the testes.
UHI / CC0
Download text version
In females FSH stimulates maturation of the follicles in the ovary and oestrogen secretion, leading to ovulation. LH triggers ovulation, and transforms the Graafian follicle into the corpus luteum.
Following the release of LH and FSH, the maturing follicle secretes oestrogen and progesterone. This initially has a negative feedback effect on FSH production, but high oestrogen levels prior to ovulation increase pituitary secretion of FSH and LH (a positive feedback effect), and FSH and LH levels peak immediately before ovulation.
Luteinising hormone and follicle stimulating hormone in the male
Gonadotrophin Releasing Hormone (GnRH) is produced in the hypothalamus and stimulates the anterior pituitary to secrete Luteinising Hormone (LH) and Follicle Stimulating Hormone (FSH). These hormones stimulate the male reproductive organs.
Luteinising Hormone in males is also called Interstitial Cell Stimulating Hormone (ICSH). This hormone stimulates the interstitial cells in the testes to produce testosterone. FSH facilitates spermatozoa production by stimulating growth of the seminiferous tubules of the testes.
The hormone Inhibin stops the release of FSH which leads to a reduction in the production of spermatozoa. This process occurs by negative feedback to the anterior pituitary gland once the required level of spermatogenesis has been achieved.
Quiz
Test yourself
Summary
You have completed your study of the Endocrine System.
You should now have a good knowledge and understanding of the anatomy and physiology of the Endocrine System. You should be able to...
- Explain how the endocrine system creates homeostasis in the body
- Identify and name the organs in the endocrine system
- Explain the role of the hypothalamus and pituitary glands
- Discuss where each hormone in the endocrine system is secreted from, its target cells and actions in the body
UHI / CC0